Have you ever read the annual Takeda Prescription Drug Benefit Cost and Plan Design Report? It is a great summary of data from 340 employers representing over 6M members and this version is based on data from May and June 2007.
Here are my notes:
- 89% use tiered formularies. [I am amazed that 11% still have a one-tier plan.]
- Closed formularies (where drugs not on the list aren’t covered at all) have almost disappeared.
- 11.1% of employers use mandatory mail.
- Mail order penetration with mandatory mail is 27.3%.
- 26.8% of employers use retail pharmacies to dispense 60+ day prescriptions.
- 51.5% of employers require use of a specific specialty pharmacy. (mandatory specialty)
- 40-70% of the specialty drug spend is under medical not pharmacy
- Flat dollar copayments still represent about 75% of plan designs
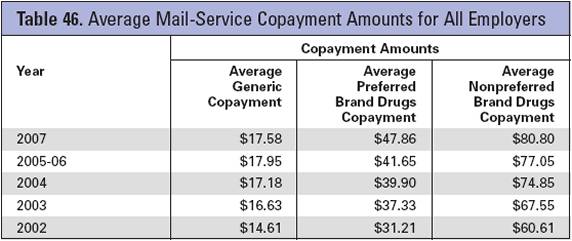
- The average copayments for retail are $8.91, $23.08, $39.77 and for mail are $17.99, $47.89, and $81.07.
- It talks a little about using lower copayments to increase adherence:
- Pitney Bowes piloted this concept which you can find out more about at the Center for Health Value Innovation.
- Other companies trying this are Marriott, P&G, and Eastman Chemical. I believe several of them are working with ActiveHealth on this.
- University of Michigan is trying a 2-year pilot for members with diabetes.
- A lot of this work is driven by the older Asheville Project.
- It also mentioned a program called HealthMapRx developed by the American Pharmacist Association (APhA) which is apparently used by 80 employers.
- The Cleveland Clinic has a plan outlined here where they dropped their statin copayments dramatically from $75 and $90 for 90-days to $6 for a generic and $8 for Lipitor or Crestor. The drugs had to be purchased from the clinic’s pharmacies. Additionally, the employee had to split the pills (i.e., get a Lipitor 40mg pill and split it to get two 20mg pills) except for those who required the highest doses.
- 38% of eligible members participated
- Adherence went up 20% in year one
- 50% of those that participated picked up all their prescriptions in year one compared with 18% of those that didn’t participate
- The average pharmacy reimbursement rates as a percentage off AWP were:
- Retail brand 16.1%
- Retail generic 43.6%
- Mail brand 22.7%
- Mail generic 51.8%
- Specialty 16.5%
- For most, they still show an average dispensing fee although I thought that was gone in mail for sure. (It says only 20% pay a dispensing fee at mail.)
- The brand rates seem pretty reasonable, but I think the generic rates are pretty pathetic. I thought it would be more like 50% retail and 60% mail.
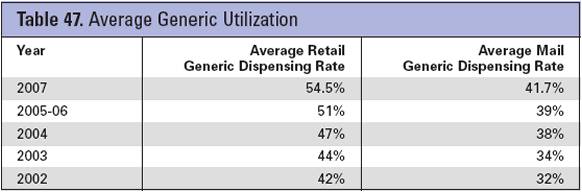
- The GFR (generic fill rate) ranged from 4.7% to 71% at retail and 1.8% to 71.4% at mail. (Note that your GFR at retail should be higher as their are more acute generics.)
- The average GFR was 54.5% retail and 41.7% mail.
- The copay differential between tiers one and three makes a difference…at least at retail (what about one and two?):
- If it is $25 or more, the retail GFR was 4.9% more and if it was $65 or more at mai, the mail GFR was 0.6% less.
- The averages for Rxs PMPM and costs were broken out by active employee and retiree:
- Rxs PMPM were 2.1 active and 3.5 retiree
- Gross costs PMPM were 76.15 active and 146.23 retiree
- Net costs PMPM were $55.52 active and $122.99 (with highest being 401.32 and 359.00)
- Rebates per branded Rx (actual not guaranteed) were:
- $2.57 retail
- $10.79 mail
- There is another case study insert about the University of Michigan’s pill splitting program for statins (aka cholesterol lowering drugs).
- Participants save 50% on copay and get a free pill splitter
- 500 people participated saving them $195,000 and the patients saved $25,000 in copays
- According to their director of benefits, if 25% of eligible statin users split pills, they could save $740,000 per year
- So, they must have had about 6% participation in the year one savings above
- I was actually shocked by the number of employers covering some OTCs (which I think is great).
- 83.9% cover Prilosec OTC
- 79.3% cover loratadine (Claritin)
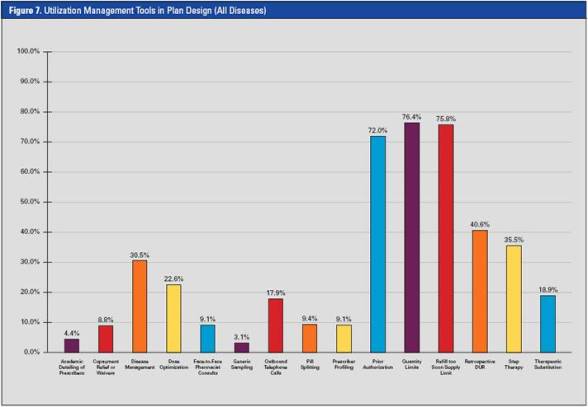
- 76.4% use some quantity level limits
- 75.8% use refill too soon logic (I thought this would be 100%)
- The classes most typically excluded from coverage

 March 14, 2008
March 14, 2008