A few weeks ago, as a follow-up to my discussion with Aetna about CarePass, I had a chance to talk with David Tripi from Janssen Healthcare Innovation about their new solution.
David is a founding partner at Janssen Healthcare Innovation where he is part of a multi-disciplinary group working toward the goal of propelling the company to become the leader in the healthcare solution business. Prior to the launch of the JHI team, David was with Johnson & Johnson for over 15 years.
“Janssen Healthcare Innovation (JHI), an entrepreneurial group within Janssen Research & Development, LLC, develops cutting-edge health solutions designed to modernize healthcare delivery, improve patient outcomes, and create a healthier world.” This is a 3-year old effort by Johnson & Johnson focused on integrated care businesses and enabling technologies. To support those, medication adherence and mobile are key areas.
One thing that David stressed is that they are platform agnostic and that their Care4Today Mobile Health Manager works as both an app and via SMS. Therefore, the 50% of the US that doesn’t have a smartphone can still use it. Additionally, it’s not a product or drug specific solution. You can use this even if you don’t use a J&J product.
Adherence is a huge challenge that everyone is aligned around, and everyone is trying to find solutions – plan design, incentives, apps, consumer engagement, framing, behavioral economics, and smart pill bottles (to name a few). So, what’s part of the Care4Today solution?
- It has reminders for Rx and OTC products.
- It has a refill reminder process which they hope to automate in the future.
- It has a two way secure messaging platform.
- It has images of over 20,000 pills.
- And, they also included a caregiver strategy and an incentive option.
The idea of social health is important. We’ve talked about this for weight loss and smoking. But, with the expanded role of caregivers, can they play a key role in improving adherence? For example, if you respond that you didn’t take your pill and the response goes to your caregiver, will they call you? Will that follow-up motivate you? (Care4Family) Some prior research says yes.
A broader question might be about how to pick a caregiver or how to define it. Should it just be your family? Should it include your physician? What if you don’t have a support system? Could the healthcare companies or advocacy companies give you a “professional caregiver”? What about an avatar as a caregiver?
I asked about the incentive program that they included (Care4Charity). David pointed out that using apps isn’t fun (at least for most people) so they wanted to give a slight motivation. I questioned him on why $0.05 (which is the daily donation if you check in and take your meds). They did lots of research which showed that the amount didn’t really matter. So, this is an experiment to see if this extra feature of the program will nudge people to be more adherent. Or ultimately, it would be great to segment the population to understand who it was motivating for and for whom it didn’t matter.
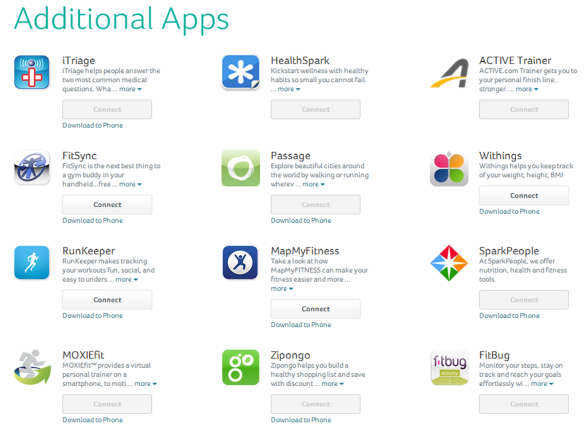
One of the things I wondered about was how they were going to promote the app. Obviously, relationships with companies like Aetna and their CarePass program are one way, but with the tens of thousands of apps out there, how will people find it? David told me that they were going to initially focus on social media – Facebook, Twitter, and mommy blogs – to drive awareness. Next, they’re going to use pharma reps to discuss the app with physicians and pilot this strategy in HIV.
At the time, they’d had over 55,000 consumer downloads, and they’ve already gotten some initial feedback from physicians that like the fact that they’re offering solutions that aren’t branded to a specific pharmaceutical product. Some of those physicians are already offering it to patients. They expect this will be a big driver. They are now starting to talk with retail pharmacies about how to encourage consumer use. While my initial reaction was that this would be “competitive” with the Walgreens and CVS Caremark mobile solutions, they see collaboration opportunities especially with Walgreens and their open API.
Of course, I wondered about how the app was being used, but they don’t collect PII (personally identifiable information). In the future, they plan to offer an option for patients to opt-in to share information and create a clinic dashboard for physicians to see which patients are using it and providing them with data. And, with a new collaboration with HealthNet, consumers will be logging into the app with their HealthNet ID which will allow them to link up PII and PHI (protected health information).
So, what’s next…
- They’ve launched in the US and France. They’re expanding into the UK and other countries next.
- They’re adding Spanish in Q1-2014.
- They’ve just completed some human factor testing which will drive some UI and UX changes.
- They’re going to do some testing and look at results with whatever data is available.
- They’re going to try to partner with as many people as possible.
Will it move the needle around adherence? It’s still too early to tell. But, it’s great to see pharma testing new strategies and working in new ways with payers to try to address this challenge.

 January 6, 2014
January 6, 2014