I’ve been closely following Aetna’s innovation for the past few years (see post on CarePass and Healthagen). I had the chance last week to speak with Adam Scott who is the Managing Director of the Aetna Innovation Labs.
Here’s Adam’s bio:
Adam Scott is a Managing Director within Aetna’s Innovation Labs, a group developing novel clinical, platform, and engagement solutions for the next generation of healthcare. Mr. Scott specializes in clinical innovation, with a focus on oncology, genetics, and metabolic syndrome, as well as “big data” analysis. His work is aimed at conceptualizing and developing products and services that better predict illness, enable evidence-based care and lengthen healthy lives. Prior to joining Aetna, Mr. Scott’s 15-year healthcare career has included management roles in consulting, hospital administration, and most recently health information technology. Mr. Scott holds a bachelor’s degree from Washington University in St. Louis and a Masters in Business Administration from Northwestern University’s Kellogg School of Management. Mr. Scott resides with his family in Needham, MA, where he actively serves as a director on community boards.
This is one of my favorite topics – Metabolic Syndrome (although yes…I still hate the term).
Definition of Metabolic Syndrome from the NIH:
Metabolic (met-ah-BOL-ik) syndrome is the name for a group of risk factors that raises your risk for heart disease and other health problems, such as diabetesand stroke.
The term “metabolic” refers to the biochemical processes involved in the body’s normal functioning. Risk factors are traits, conditions, or habits that increase your chance of developing a disease.
The Aetna Innovation Labs are focused on bringing concepts to scale and staying 2-3 years ahead of the market. They are looking to rapidly pilot ideas with a focus on collecting evidence. In general, Adam described their work as focused on clinical, platform, and engagement ideas. They are trying to collaborate with cutting edge companies that they think they can help to scale quickly. It’s pretty exciting!
As stated in their press release about this new effort:
“During the course of the last year, Aetna Innovation Labs has successfully piloted an analysis of Metabolic Syndrome and the creation of predictive models for Metabolic Syndrome. This prior work showed significantly increased risk of both diabetes and heart disease for those living with Metabolic Syndrome,” said Michael Palmer, vice president of Innovation at Aetna. “With this new pilot program with Newtopia, we are aiming to help members address Metabolic Syndrome through specific actions, before more serious chronic conditions arise, like diabetes and heart disease.”
Aetna selected Newtopia for this effort for their unique approach toward achieving a healthy weight with an integrative and personalized focus on nutrition, exercise, and behavioral well-being. Newtopia’s program begins with a “genetic reveal,” leveraging a saliva-based genetic test to stratify participants with respect to three genes associated with obesity, appetite, and behavior. Based on the results of this test and an online assessment, Newtopia matches each participant to a plan and coach trained to focus on the member’s specific genetic, personality and motivation profile. Through online coaching sessions, Newtopia will help members achieve results related to maintaining a healthy weight and Metabolic Syndrome risk-reduction, which will be measured by changes from a pre- and post-program biometric screening.
“Newtopia’s mission is to inspire individuals to make the lifestyle choices that can help them build healthy lives,” said Jeffrey Ruby, Founder and CEO of Newtopia.
If you’ve been following the story, this builds upon their project with GNS to develop a predictive algorithm to identify people at risk for Metabolic Syndrome. As you may or may not know, there are 5 first factors for Metabolic Syndrome (text from NIH):
The five conditions described below are metabolic risk factors. You can have any one of these risk factors by itself, but they tend to occur together. You must have at least three metabolic risk factors to be diagnosed with metabolic syndrome.
-
A large waistline. This also is called abdominal obesity or “having an apple shape.” Excess fat in the stomach area is a greater risk factor for heart disease than excess fat in other parts of the body, such as on the hips.
-
A high triglyceride level (or you’re on medicine to treat high triglycerides). Triglycerides are a type of fat found in the blood.
-
A low HDL cholesterol level (or you’re on medicine to treat low HDL cholesterol). HDL sometimes is called “good” cholesterol. This is because it helps remove cholesterol from your arteries. A low HDL cholesterol level raises your risk for heart disease.
-
High blood pressure (or you’re on medicine to treat high blood pressure). Blood pressure is the force of blood pushing against the walls of your arteries as your heart pumps blood. If this pressure rises and stays high over time, it can damage your heart and lead to plaque buildup.
-
High fasting blood sugar (or you’re on medicine to treat high blood sugar). Mildly high blood sugar may be an early sign of diabetes.
So, what exactly are they doing now. That was the focus of my discussion with Adam.
- They are running data through the GNS predictive model.
- They are inviting people to participate in the program. (initially focusing on 500 Aetna employees for the pilot)
- The employees that choose to participate then get a 3 SNP (snip) test done focused on the genes that are associated with body fat, appetite, and eating behavior. (Maybe they should get a few of us bloggers into the pilot – hint.) This is done through Newtopia, and the program is GINA compliant since the genetic data is never received by Aetna or the employer.
- The genetic analysis puts the consumer into one of eight categories.
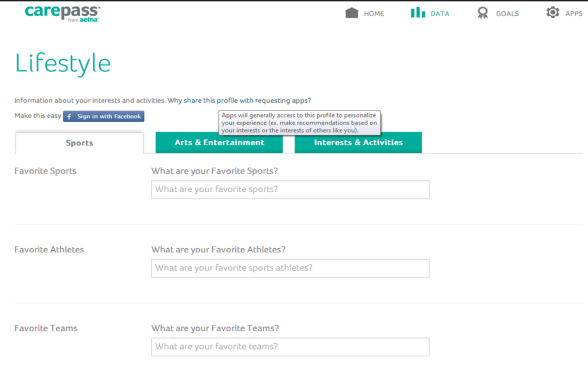
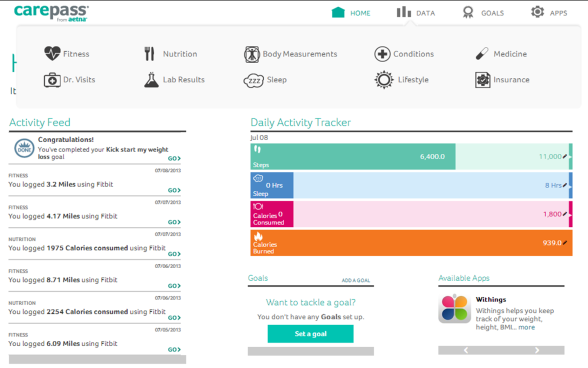
- Based on the category, the consumer is matched with a personal coach who is going to help them with a care plan, an exercise plan, and a nutrition plan. The coaching also includes a lifestyle assessment to identify the best ways to engage them and is supported by mobile and web technology.

- The Newtopia coaches are then using the Pebble technology to track activity and upload that into a portal and into their system.
We then talked about several of the other activities that are important for this to be successful:
- Use of Motivational Interviewing or other evidence-based approaches for engagement. In this case, Newtopia is providing the coaching using a proprietary approach based on the genetic data.
- Providing offline support. In this case, Aetna has partnered with Duke to provide the Metabolic Health in Small Bytes program which he described as a virtual coaching program.
Metabolic Health in Small Bytes uses a virtual classroom technology, where participants can interact with each other and the instructor. All of the program instructors have completed a program outlined by lead program developer Ruth Wolever, PhD from Duke Diet and Fitness Center and Duke Integrative Medicine. Using mindfulness techniques from the program, participants learn practices they can use to combat the root causes of obesity. The program’s goal is to help participants better understand their emotional state, enhance their knowledge of how to improve exercise and nutrition, and access internal motivation to do so. (source)
We also talked about employer feedback and willingness to adopt solutions like this. From my conversations, I think employers are hesitant to go down this path. Metabolic Syndrome affects about 23.7% of the population. That is a large group of consumers to engage, and pending final ROI analysis will likely scare some employers off.
Adam told me that they’ve talked with 30 of their large clients, consultants, and mid-market clients. While we didn’t get into specifics, we talked about all the reasons they should do this:
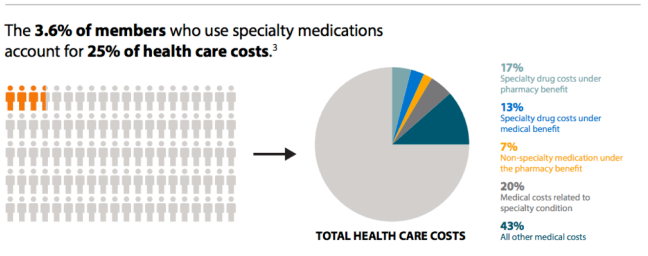
- People with Metabolic Syndrome are 1.6x more expensive
- People with Metabolic Syndrome are 5x more likely to get diabetes
- Absenteeism
- Presenteeism
This ties well with my argument that wellness programs aren’t just about ROI.
Obviously, one of the next steps will be figuring out how this integrates into their other existing programs to address the overall consumer experience so that it’s not just another cool (but disconnected) program. And, of course, to demonstrate the effectiveness of the program to get clients and consumers to participate.
Two quotes I’ll leave you with on why this is difficult (but yet exciting to try to solve):
“The harsh reality is that scientists know as much about curing obesity as they do about curing the common cold: not much. But at least they admit their limitations in treating the cold. Many doctors seem to think the cure for obesity exists, but obese patients just don’t comply. Doctors often have less respect for obese patients, believing if they would just diet and exercise they’d be slim and healthy.” (source)
Thirty percent of those in the “overweight” class believed they were actually normal size, while 70% of those classified as obese felt they were simply overweight. Among the heaviest group, the morbidly obese, almost 60% pegged themselves as obese, while another 39% considered themselves merely overweight. (source)

 September 2, 2014
September 2, 2014