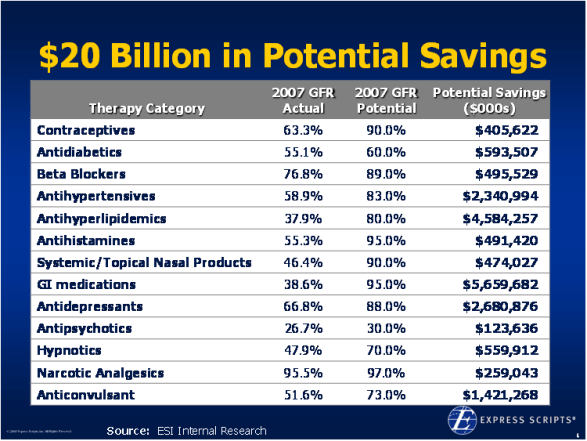
From the Express Scripts Outcomes event a few weeks ago, here is an estimate of all the money left on the table by not increasing your generic fill rate in certain key categories. Are you doing enough?
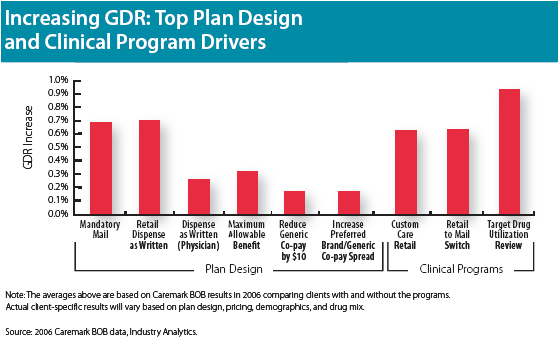
- Utilization management programs – step therapy, prior authorization, quantity level limits?
- Formulary coverage?
- Plan design incentives?
- Pharmacy incentives?
- eRx messaging?
- Web tools?
- Patient communications?
- Patient incentives?
- Driving people to mail?
Here is a graph from CVS/Caremark‘s trend report from last year that shows correlation between certain programs and generic fill rate.

 May 13, 2008
May 13, 2008 


No comments yet... Be the first to leave a reply!