[Note: I’m republishing a few Deloitte blogs that they are no longer hosting as part of the new website.]
Originally Posted by George Van Antwerp on September 28, 2017
A flying car that conveniently folds into a briefcase never materialized, but the digital revolution now underway in pharmacy could lead to a reality not far from the futuristic world envisioned by The Jetsons cartoon series of the 1970s.
As an industry, health care is often seeking ways to pay for and reward value rather than volume. While pharmacy often lags behind medical in this area, discussions are starting to focus more on consumer engagement, patient satisfaction, clinical outcomes, and collaboration across the ecosystem (i.e., retail, mail, and specialty pharmacies, distributors, manufacturers, and pharmacy benefit managers (PBMs)). Rather than creating value through scale to drive price negotiations, three primary forces will likely push companies across the pharmacy ecosystem to transform their business models:
- Advancing technologies from the Internet of Things (IOT) to Artificial Intelligence (AI).
- Growing expectations from consumers as other industries embrace them and make them the focus of their outside-in redesign of processes and technology.
- Increasing data availability and technology that leads to new insights and predictive models that allow companies to personalize and engage with consumers (and their care teams) in new ways.
If we look to the future, will pharmacy companies be the delivery channel, the aggregator, the clinical care management company, the technology vendor or something very different? As pharmacy leaders ask themselves where they want to play and how they will win, defining the role of pharmacy within the health care ecosystem will likely be critical.
Technology: Imagine the following future scenario (all of which is in development).
As you start your day, your smart toilet detects abnormal sugar levels in your urine and alerts your physician. After a telehealth visit (from your couch) with an avatar of your physician, your physician gives you a prescription for a new medication. You fill your own prescription using a 3D printer. The generic drug is embedded with a smart chip that transmits clinical data back to the physician before dissolving in your stomach. The physician sends information about common side effects to your home monitoring system, which tracks your health and compliance. After a few days, your smart home recognizes you as you walk into the kitchen and asks how you are feeling. Your response about a rash correlates with a common side effect, and the monitoring system offers to schedule an appointment with your physician to determine if an alternative medication might be better.
While none of these technologies will see broad adoption any time soon, the pharmacy industry should consider investments now in preparation for the future. Such investments will likely help traditional players compete with start-ups and health-focused technology companies that will probably try to carve out the most profitable sectors (as we see in retail).
Pharmacy companies should be asking:
- How should we work with smart devices and use that data to help manage conditions such as diabetes?
- How can we more effectively share data and clinical insights with physicians?
- How should we collaborate with pharmaceutical manufacturers to think about drug delivery and real-world evidence?
- How can we use artificial intelligence and predictive models to enhance the customer experience?
- How can we help consumers save time and money?
- How can we simplify health care to improve engagement, adherence, compliance, and outcomes?
Consumerism: Today’s hypercompetitive marketplace often requires constant innovation and digitization. It commonly requires companies to look at their products and solutions through the eyes of the consumer, particularly as adoption of high-deductible health plans (HDHPs) continues to expand. One way to think about this is to follow the consumer journey. Here are four moments when consumers are often open to engagement:
| Open Enrollment | What is the best health plan for me given my conditions and prior medication use? How can I save money? What is the likely progression of my condition? |
| Diagnosis | What is wrong with me? What are my treatment options? How have other patients responded to this medication? What are the side effects? Is there a lower-cost medication? |
| Pharmacy Selection & Pick-up | Which pharmacy will save me the most money? Which pharmacy is most convenient? Where will I get the best service? What do I need to know about the drug and my condition? Will it interact with any food I eat, vitamins I take, or other medication? What is this prior authorization and why did I not know about it until I went to pick up my medication? |
| Ongoing Support & Management | What should I be doing to manage my condition? Why was my copayment so high? How can I see the status of my order in real-time through an app? How do I know if the medication is working? Am I better or do I have to keep taking the medication? |
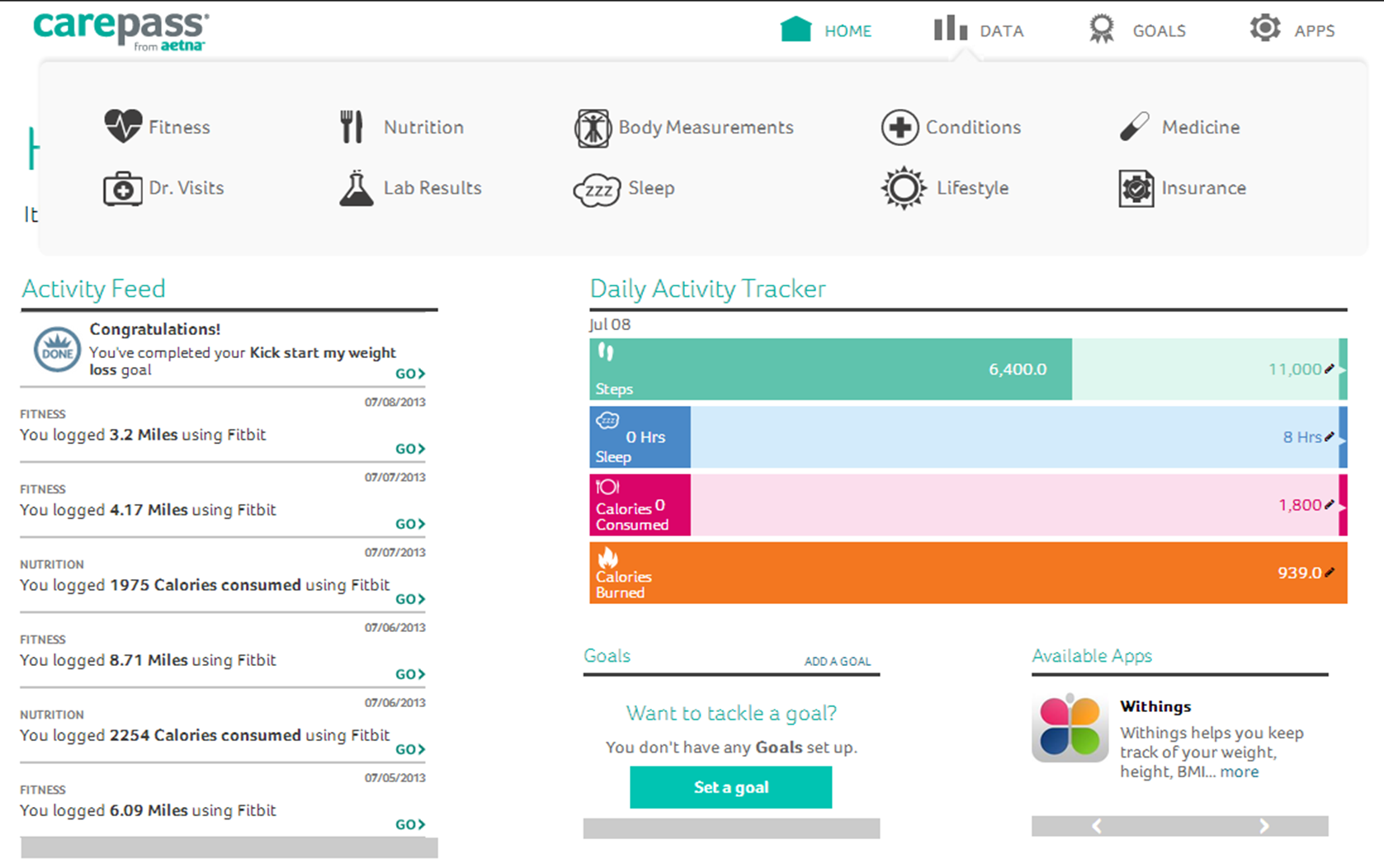
Data: For many companies, it is still a challenge to integrate pharmacy and medical data. When you begin to look at lab data and unstructured data (e.g., patient reported outcomes, physician notes), the challenge can increase. At the same time, many technologies are creating new opportunities to leverage data and analytics to shift from reactive to proactive.
Data and analytics might help the pharmacy industry to:
- Predict who will be adherent to a medication, and match that patient to an intervention.
- Create a risk score around abuse that identifies at-risk patients and triggers an earlier intervention.
- Develop a churn model that determines which patients are likely to switch pharmacies, and offer insight into how to retain them.
- Create a one-to-one marketing approach to determine the right message in the right channel to the right person at the right time going beyond segmentation and personas.
- Identify and route an inbound caller to the most appropriate agent using a predictive reason code.
- Identify patients at risk for depression so that their treatment can be managed effectively.
Three drivers of change – technology, consumer, and data – will likely manifest themselves in different ways at different companies. As leaders think about business-model innovation and new product solutions using frameworks such as the Ten Types of Innovation or the Ambition Matrix, we will likely continue to see greater differentiation across the pharmacy market. I am excited about what this means for pharmaceutical manufacturers, wholesalers, PBMs, retail pharmacies, specialty pharmacies, and provider owned pharmacies.
This blog was first published in A view from the Center: Deloitte’s Life Sciences & Health Care Blog

 February 13, 2021
February 13, 2021