While I’ve moved most of the infographics I find to my Pinterest account, I wanted to capture and share this one from Stephen Wilkin’s blog since it hits so many of the points that I try to make with people.
The Role Of Healthcare Technology Curator
When I worked as an IT consultant, you had two clear choices – an enterprise system (e.g., SAP) or a best-of-breed (BOB) strategy. People liked the simplicity of an enterprise system, but you may have sub-optimized reporting or some flexibility in your solution. On the other hand, the BOB strategy required more maintenance, effort, and coordination to pull it off in a coordinated fashion.
In today’s healthcare world, I look at and meet with a ton of technology companies. The struggle is how to keep up with all the change in the industry and be nimble enough to engage the new start-up, but flexible enough to evolve with the market without impacting the consumer experience.
Maybe it draws on my training as an architect, but I was describing my technology vision as one of a general contractor. The buyer (client) wants a BOB solution. They want everything optimized – data, reporting, workflow, content, mobile, clinical algorithms, etc. At the same time, they often underestimate what it takes to manage all of these vendors, integrate the data on the backend, and create an integrated consumer experience across multiple vendors and technology platforms.
That’s where I see some real value add as a “technology curator”. I see one of my roles in helping manage an evolving ecosystem of healthcare companies and working with a flexible technology platform that can quickly plug and play with different solutions. This also allows me to have pre-built integrations with certain solutions, but I can also offer consumers the ability to choose their device (for example) and with the right API set up just be device agnostic in my solution.
Over time, this offers clients a lot of flexibility. The get the BOB approach within an enterprise system environment. They don’t have to keep issuing RFPs and evaluating vendors (since we’re doing that). They don’t have to stitch together multiple data sets to create the integrated, longitudinal view of the consumer (since we’re doing that). They don’t have to pretend that they’re offering a cohesive consumer experience (since we’re doing that). And, most importantly, they are flexible over time to jump from solution to solution within the architecture without disrupting everyone since it’s behind the “presentation layer” that the consumer experiences.
MTM is like Population Health Management
I saw this quote of the day in Drug Benefit News, and it made me think about all the discussions I’ve been having around population health management and the need for a longitudinal patient record and integrated member experience.
Medication therapy management (MTM) at its core is viewing “the member in its entirety and not as individual activities…and looking at all of those things around medications for that patient. You can have the best programs in the world but if the patient is not engaged, they are a waste of time and energy, and that’s why an integrated activity like MTM has the opportunity to be so significantly effective.”
– Jan Berger, M.D., chief medical officer at Silverlink Communications, Inc.
Click here to read the DRUG BENEFIT NEWS article in which this quote appeared.
The #QuantifiedSelf and “Walking Interview”
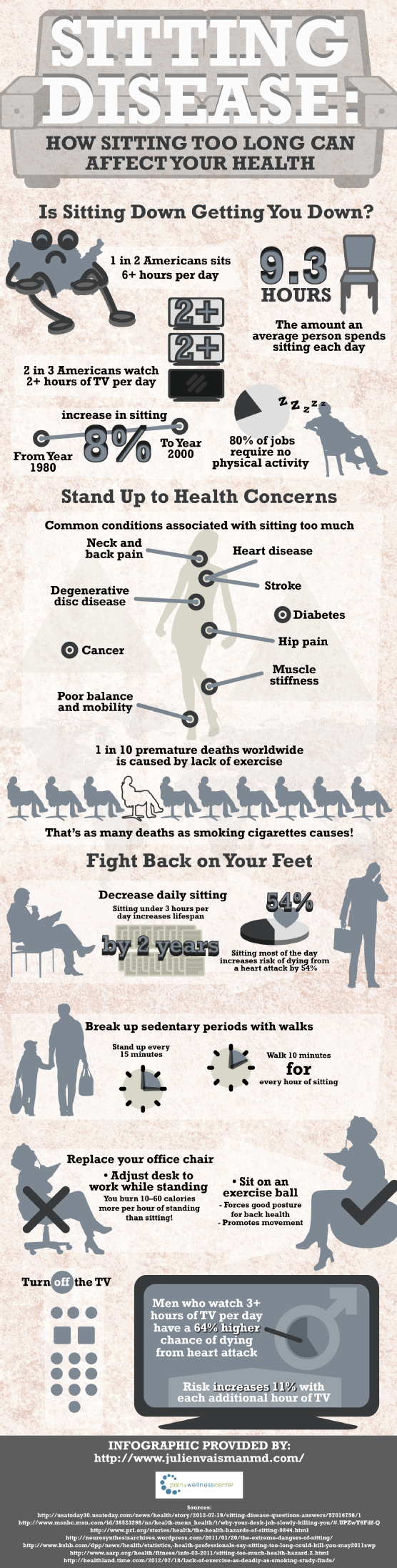
If you haven’t heard, “sitting is the new smoking” in terms of health status. And, unfortunately, you can’t just get up and exercise for an hour and then go sit all day. That brief spurt of exercise doesn’t change the fact that we sit for 9+ hours a day.
If you think about our shift in work from a very manual work environment to a service and technology work environment, we’ve made activity during the day harder and harder to achieve. Between e-mail and meetings, most of us are stagnant to accomplish our work.
That got me thinking about the #QuantifiedSelf movement and all of the activity trackers (e.g., FitBit, BodyMedia). We know companies definitely look online to see people’s social media activity as part of the interview process. Will they begin to ask about their activity data as a proxy for health?
On the flipside, perhaps the person interviewing should really be asking to see their potential boss’ activity data. I’d be as interested in knowing what happens during the day. It would provide a lot of insight into what happens in terms of meetings, face-t0-face activity, and be a good proxy for the real work experience.
Of course, the other option would be to introduce “walking interviews”. People talk about walking meetings. I’ve even done a running meeting going for a jog with a potential partner to discuss how we work together. (It was the only time we could find to meet at a conference.)
Walking interviews would tell you a lot about someone’s health. You could go up some stairs. You could walk a few miles in an hour.
Since we know that health, happiness, and wealth are all correlated, this type of insight for the interviewer and interviewee seems very valuable.
Could Generic Prescriptions Be The Greatest Placebo Ever?
Those of you who know me know that I’ve been a huge advocate for generic prescriptions since the early part of my PBM/pharmacy career in 2001. It wasn’t long ago that I talked about unresponsible reporting when slamming generics and scaring the population. But, we all enjoy a good conspiracy theory which is about the only thing that makes sense reading the new Fortune article – Dirty Medicine – about Ranbaxy. Both articles are written by the same author, but this one scares me a lot more than the other one. This article reads like a fiction book but appears to be true. It should scare you also and put a spotlight on the FDA.
Here are a few things from the article.
On May 13, Ranbaxy pleaded guilty to seven federal criminal counts of selling adulterated drugs with intent to defraud, failing to report that its drugs didn’t meet specifications, and making intentionally false statements to the government. Ranbaxy agreed to pay $500 million in fines, forfeitures, and penalties — the most ever levied against a generic-drug company.
The company manipulated almost every aspect of its manufacturing process to quickly produce impressive-looking data that would bolster its bottom line. “This was not something that was concealed,” Thakur says. It was “common knowledge among senior managers of the company, heads of research and development, people responsible for formulation to the clinical people.”
It made clear that Ranbaxy had lied to regulators and falsified data in every country examined in the report. “More than 200 products in more than 40 countries” have “elements of data that were fabricated to support business needs,” the PowerPoint reported. “Business needs,” the report showed, was a euphemism for ways in which Ranbaxy could minimize cost, maximize profit, and dupe regulators into approving substandard drugs.
But, we know that generics have worked. People have gotten better so one has to assume this isn’t a massive fraud especially when 50% of generics have traditionally been made by the brand manufacturers themselves who would never risk their companies to do what Ranbaxy did. So, it made me wonder about the Placebo Effect. Did some drugs work simply because of that? Is there anything else that would make sense for why this wasn’t discovered more quickly?
I’ve talked a lot about the Placebo Effect. There’s now even an app to make you feel better using the Placebo Effect.
- https://georgevanantwerp.com/2013/01/15/saturday-evening-post-on-the-placebo-effect/
- https://georgevanantwerp.com/2008/10/25/prescribing-placebos/
- https://georgevanantwerp.com/2008/03/08/does-price-have-a-placebo-effect/
I’m shocked that the PBMs, pharmacies, manufacturers, associations, wholesalers, and others aren’t out talking about this. I would want to let the public know that this isn’t a systemic problem, but is one contained to one instance and that quality will be maintained…but maybe no one cares?
Relocation vs. Travel – Presenteeism and Health Implications
Surprisingly, I’ve been happily living in the St. Louis area for almost 20 years. I moved here after going to the University of Michigan for graduate school at Washington University, and I never thought I’d stay. My girlfriend (now wife) moved a year later, and we’ve loved it ever since. We’ve built two houses, had two kids, and made a lot of friends.
I’ve had chances to move many times to Kansas City, San Francisco, Boston, Columbia (SC), Florida, Minneapolis, New York, New Jersey, and several other cities. All of them I have turned down. So, one of the big questions I get asked now days is why are you moving out of St. Louis since you’ve commuted for so long and “enjoyed” it. That’s a tough one, but as someone who cares about my health, let me position this from a health perspective for all of you.
Ultimately, we’re moving for one reason which is to spend more time with my family. Of those 20 years, I estimate that I’ve spent at least 9 of them where I traveled 50-90% of the business days. You can do the math, but if I assume 15 days per month on the road over 9 years, that’s about 1,620 days that I’ve been gone or 4.4 years. That’s a lot of time to miss with your wife and kids.
But, I also see several health reasons for this:
- Most people I know (including myself) sleep better at home and have a more regular routine. No early morning flights. No late night flights. No uncomfortable beds. No loud neighbors. No temptation to work until all hours of the night. And, as I’ve talked about many times, lack of sleep is a major contributor to productivity, decision making, and health.
- You eat better at home and don’t have to eat out every meal which can affect your calorie intake and therefore your weight.
- Long commutes have both mental and physical health implications (none of them good) as you can see in this article and infographic on LifeHacker along with this other article on ABC.
- Being at home and spending time with your family can also affect them (as we know health is social). Here’s one example about eating with your kids that I often quote.
Of course, commuting has some productivity gains (if done right) from a work perspective:
- You can work long days without worrying about other things that you should do when you’re home. (Why do you think consultants are so productive?)
- You can find some nice quiet time on planes to work. (Although this has gone down over time with more crowded flights, more connecting flights, and smaller seats.)
You have to trade this off with productivity lost on travel days (e.g., I wake up every Monday at 4:30, leave for the airport at 5:30, land in Charlotte at 10:15, and get to my office around 11:30 with best case 90 minutes of work done).
But, moving definitely impacts your presenteeism as I’m learning (at least for a few months). After 20 years in one city, there’s a lot to do to move. You have to find new service providers (doctors, dentists, handyman, vet, hair), new schools, new sports teams, new stores, etc.
But, for those of you that aren’t convinced since you think travel is glamorous, let me share just a few stories with you.
- On one of my toughest travel days, I had breakfast with a CIO in Boston at 6:30 am; caught a flight to Minneapolis to give a presentation over lunch; then caught a flight to have a dinner meeting in San Francisco. Long day.
- In some weeks, I used to spend over 20 hours a week in a plane (not including airport time). Talk about sitting disease.
- Just yesterday, when I tried to squeeze in one last trip before I moved, I got up at 3:30 to catch a 6:00 flight. I flew to Florida took a few calls, had a meeting, and then came back to the airport to catch an 8:oo PM flight home. That flight was delayed until 2:05 AM meaning that if I hadn’t just gone to get a hotel room (without any clothes or toiletries) that I would have gotten home 24 hours after I left the house.
Of course, the frequent flyer miles and hotel points are great. We’ve taken many a trip with it. I’ve given my parents free flights. Heck, we’ve even given our dog walkers free flights.
The key is to evaluate several factors which are what I’ve looked at:
- Will you be traveling from which ever city you live in? Don’t move your family just to be traveling out of a new city.
- Do you like the new city and would you consider living there long-term? For example, I know I probably would never like true city living in NY.
- What is important to your family and is it present in the new city? This is a complicated one to find the right mix of services and education.
- Can you afford to live in the new location without a major impact on your quality of life (or will your job account for this)?
Anyways, this has been one reason why I haven’t been blogging as much lately. The move is all consuming especially with lots of things going on at work. I have 4 more days in St. Louis before moving so we’re excited and nervous.
Personalized and Relevant Messages are Key to Successful Patient Engagement
Guest Post From The President of TeleVox Software
It shouldn’t come as a surprise to anyone that we live in a society yearning for instant gratification. We expect to get information in the blink of an eye, the answers we need within minutes and material goods delivered prior to the date that was promised. But what may surprise you is that even through the desire to have this information so quickly, the importance of providing a personalized message remains one of consumers’ biggest wishes. For instance, studies show that tailoring the message to the needs of patients as well as personalizing the messages are key to successful high-tech patient engagement. In fact, according to a recent TeleVox Healthy World Report, Technology Beyond the Exam Room: How Digital Media Is Helping Doctors Deliver the Highest Level of Care, 50 percent of patients expect information to be personalized to their specific needs. In the age of instant feedback and heightened technology, it is interesting to know that patients still desire a personalized approach in terms of their healthcare.
The days of simply setting forth wellness plans based solely on numbers and stereotypes are past us. Patients are looking for communications that are relevant to their lives, and it is their expectation that healthcare professionals will take time to engage in this level of personalization. Know Your Health also found that 53 percent of patients expect communications to be relevant to them as individuals. Relevant patient engagement can include personalized interactions, individualized treatment plans, and follow up. Patients thrive on a feeling of importance, ranging from a doctor knowing their name and medical history when they walk in to a follow-up call or email after the appointment to continue that personal connection.
Think about this: According to the same report, 21 percent of the population will refuse information if it is not tailored specifically to them. And, further, 13 percent of patients surveyed report they will ignore information sent their way if it doesn’t have their name on it. Why would providers want to miss out on connecting with an important part of the population by simply not including their name on any communication to the patient? Including this step can ensure patient engagement is successful and save valuable resources, as the information conveyed will have a better chance of being received by patients.
Finally, taking time to connect with patients outside of their yearly exams or scheduled check-ups is another important link in ensuring that patients make positive decisions that ensure a healthy future. 68 percent of the population would like to receive educational tips that will help them live a better life via email throughout the year. Many Americans are concerned with the direction of the overall health and well-being of the country, but still aren’t taking steps to get where they need to be. However, healthcare providers can take steps to tailor messages that are relevant and personalized to patients to ensure successful high-tech patient engagement, and ultimately a healthier America.
Scott Zimmerman is a regularly-published thought leader on engaging patients via ongoing communication between office visits. He is the President of TeleVox Software, Inc, a high-tech Engagement Communications company that provides automated voice, email, SMS and web solutions that activate positive patient behaviors by applying technology to deliver a human touch. Scott spearheads TeleVox’s Healthy World initiative, a program that leverages ethnographic research to uncover, understand and interpret both patient and provider points of view with the end goal of creating a healthy world–one person at a time. Zimmerman possesses 20 years of proven performance in the healthcare industry, with domain knowledge in the surgical, interventional and pharmaceutical arenas. Prior to joining TeleVox, Scott served for nine years at GE Healthcare in a variety of cross-functional and global leadership roles in sales, services, quality, marketing, pricing, finance and product development. Scott is a graduate of the John M. Olin School of Business at Washington University in St. Louis.
Why Do People Think Adherence Is So Easy?
I think we all know that medication adherence is a big deal. The most common number quoted is the $290B waste number from NEHI. There are numerous studies that confirm the value of non-adherence even one that just came out.
The amount of money spent on trying to improve adherence is huge! Pharma has worked on. Retail pharmacies have worked on it. Providers have worked on it. Insurance companies have worked on it. Employers have worked on it… And all of these have happened across the world.
At the same time, you see people get so excited about things don’t make any sense to me.
Let me take an easy example. A few months ago, a company called MediSafe put out a press release around moving medication adherence on statins up to 84.25%. Nothing against the company, but I read the press release and reached out to them to say “this is great, but it’s only 2 months of data…most people drop therapy after the first few months so who care…call me back when you get some good 12 month data.”
But, a lot of people got all excited and there was numerous press about this – see list of articles about them.
Now, tonight, I see another technology getting similar excitement. Fast Company talks about the AdhereTech technology which integrates a cellular phone with a pill bottle. And, it costs $60 a month. In my experience, companies wouldn’t even spend $2 a month to promote adherence so $60 is just impractical. The argument is that this is good for high cost specialty drugs that are oral solids not injectables. But, this isn’t a new idea. Glowcaps already built this model with a very slick interface and workflow.
And, I don’t know about you, but I think this would be obnoxious. And, I love data and am part of the QuantifiedSelf movement. I’m not sure I understand the consumer research here. I would have to believe all of the following to buy into this model.
- Non-adherence people are primarily not adherent due to no reminders to take their medication on a daily basis.
- People with chronic conditions that require high cost specialty drugs are going to change behavior because some bottle sends them a text message.
- Manufacturers or some other healthcare company is willing to pay $60 a month for this service.
- There won’t be message fatigue after a few months (weeks) of messaging.
- Pharmacies would be have to be willing to change their workflow to use these bottles.
Yes. Will this work for some people…sure. But, if it helps 10% of people, then my cost is really $600 per success.
Should we be working on better solutions to address adherence…of course.
But, let’s stop trying to figure out some gimmick to fix adherence. Let’s look at root cause.
For example:
- People don’t know why they’ve been given a medication.
- People don’t understand their disease.
- People can’t afford their medication.
- People don’t know what to expect in terms of side effects.
- People don’t see value in improving adherence.
- People don’t know they have to refill their medications.
- People aren’t health literate.
We have a lot of problems.
Presidential Physical Fitness Award – Reasonable? Role Models?
I must admit that I don’t remember taking the presidential fitness test as a kid. With that being said, I was surprised to learn from my daughter that in her class of club soccer, volleyball, and baseball players she was the only kid to meet the highest level (greater than the 85th percentile across several measures). She made it today by running her mile in 7:37.
So, what does this require? It made me curious. Here’s what you have to do:
Could you do that? These seem pretty difficult to me. I could probably do the mile in 6:06, but I doubt I could do 53 pull-ups. And, I doubt I could sit and reach 7 inches beyond my toes. (Looking at the 17 year old male standards.)
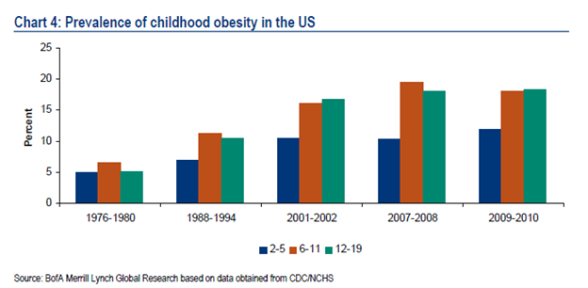
On the other hand, we certainly need our kids to be more fit. We have a big childhood obesity issue.
But, it also made me think about Michelle Obama’s efforts in this space.
I think these programs are good starts, but lets not forget that obesity is a social issue and kids learn from those around them. Let me ask the uncomfortable questions about those who our kids look up to.
- How many overweight coaches do you know?
- How about overweight teachers?
- How about policemen and firefighters?
- How about clergy?
These are all key role models…not to mention us parents who are often overweight.
I guess my suggestion here to the President would be to think about how to use our massive government payrolls as a foundation for change. Let’s think about the Presidential Fitness Challenge and create a broader wellness solution to change the visual role models for our kids and figure out how to help companies invest in this.
For example, we know that sleeping is correlated to weight and health. I was talking to my brother-in-law who is a police officer when he told me that they are expected to get 8 hours of sleep a night. Imagine if companies set this expectation for their employees (sleep impact on work).
“Sitting Disease” may make a great late night comedy story line, but it’s a reality of our information economy that has to be addressed.
How Walgreens Became One Of The More Innovative Healthcare Companies
While we are generally a society focused on innovation from start-ups (and now all the incubators like Rock Health), there are a few big companies that are able to innovate while growing. That’s not always easy and companies often need some catalyst to make this happen. Right now, there are four established healthcare companies that I’m watching closely to track their innovation – Kaiser, United/Optum, Aetna, and Walgreens. (Walgreens has made the Fast Company innovation list 3 of the past 4 years.)
I think Walgreens is really interesting, and they did have a great catalyst to force them to really dig deep to think about how do we survive in a big PBM world. It seems like the answer has been to become a healthcare company not just a pharmacy (as they say “at the corner of Happy and Healthy”) while simultaneously continuing to grow in the specialty pharmacy and store area.
Let’s look at some of the changes they’ve made over the past 5 years. Looking back, I would have described them as an organic growth company with a “not-invented-here” attitude. Now, I think they have leapfrogged the marketplace to become a model for innovation.
- They sold their PBM.
- They re-designed their stores.
- They got the pharmacist out talking to people.
- They got more involved with medication therapy management.
- They increased their focus on immunizations increasing the pharmacists role.
- They formed an innovation team.
- They invested heavily in digital and drove out several mobile solutions including innovations like using the QR code and scanning technology to order refills.
- They’ve reached out to partner with companies like Johns Hopkins and the Joslin Diabetes Centers.
- They increased their focus on publications out of their research group to showcase what they could do.
- They started looking at the role the pharmacy could play and the medications played in readmissions.
- They partnered with Boots to become a much more global company.
- They offered daily testing for key numbers people should know like A1c and blood pressure even at stores without a clinic.
- They created an incentive program and opened it up to link to devices like FitBit.
- They partnered with The Biggest Loser.
- They increased their focus on the employer including getting into the on-site clinic space.
- They created 3 Accountable Care Organizations.
- They partnered with Novartis to get into the clinical trials space.
- They developed APIs to open their system up to developers and other health IT companies.
- They formed a big collaboration with AmerisourceBergen which if you read the quote from Greg Wasson isn’t just about supply chain.
“Today’s announcement marks another step forward in establishing an unprecedented and efficient global pharmacy-led, health and wellbeing network, and achieving our vision of becoming the first choice in health and daily living for everyone in America and beyond,” said Gregory Wasson, President and Chief Executive Officer of Walgreens. “We are excited to be expanding our existing relationship with AmerisourceBergen to a 10-year strategic long-term contract, representing another transformational step in the pharmaceutical supply chain. We believe this relationship will create a wide range of opportunities and innovations in the rapidly changing U.S. and global health care environment that we expect will benefit all of our stakeholders.”
- They jumped into the retail clinic space and have continued to grow that footprint physically and around the services they offer with the latest jump being to really address the access issue and help with chronic conditions not just acute problems.
“With this service expansion, Take Care Clinics now provide the most comprehensive service offering within the retail clinic industry, and can play an even more valuable role in helping patients get, stay and live well,” said Dr. Jeffrey Kang, senior vice president of health and wellness services and solutions, Walgreens. “Through greater access to services and a broader focus on disease prevention and chronic condition management, our clinics can connect and work with physicians and other providers to better help support the increasing demands on our health care system today.” (from Press Release)
This is something for the whole pharmacy (PBM, pharma, retail, mail, specialty) industry to watch and model as I talked about in my PBMI presentation (which I’m giving again tomorrow in Chicago). It reminds me of some of the discussions by pharma leaders about the need to go “beyond the pill”.
How Aetna’s Pivoting With Healthagen – #whcc13
Do you know the term “pivot“? It’s all the rage now in terms of describing how companies continue to evolve their models with this rapidly changing business environment.
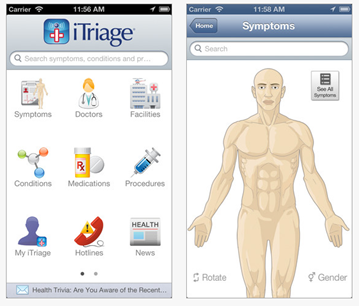
Of course, Aetna is one of the big healthcare players in the US. They’re not going to abandon a model that’s been working for well over 100 years. But, thanks to some great leadership from people like Mark Bertolini, CEO of Aetna, they’ve created a new business unit called Healthagen (building on the company they bought known mostly for iTriage). The screen shot says it all.

I got the privilege to sit down with Dr. Charles Saunders who runs Healthagen at the World Healthcare Congress in DC (#whcc13).
Charles E. Saunders, M.D., is responsible for leading the strategic diversification of Healthagen’s products, services and global opportunities. He focuses on identifying new growth opportunities and developing market strategies that can help Healthagen and Aetna profitably manage quality and cost for its customers.
Prior to joining Healthagen, Dr. Saunders served as executive in residence at Warburg Pincus, one of the world’s largest and oldest private equity firms. He has held a number of other significant leadership positions during his career, including CEO of Broadlane, Inc., President of EDS Healthcare Global Industry Solutions; Chief Medical Officer of Healtheon / WebMD; Principal of A.T. Kearney; and Executive Director of San Francisco General Hospital Managed Care Programs.
Dr. Saunders received a B.S. in biological sciences from the University of Southern California and an M.D. from Johns Hopkins University. He is board certified in Internal Medicine and Emergency Medicine and has served on the faculty of several universities, including the University of California, San Francisco; Vanderbilt University; and University of Colorado.
I also got to hear him speak right before I talked to him. (As a side note, he is a great presenter which is something that I really respect in a world of people who present too many slides, use notes, talk to the screen, and can lose you quickly.)
He hit on several key themes in his presentation that we then discussed further face-to-face:
- Social Caregiver Model
- Game Theory
- Digital / Mobile
One of my first questions was to really understand Healthagen and what it was set up to do. (As you can see from the screen shot below, they’re doing lots of things in this group.)

He boiled it down nicely to three things:
- Physician (provider) enablement
- Patient engagement
- Population Health Management IT
Our next discussion was really around why and how to create and innovate within a large company like Aetna. He reiterated what I believed that Mark Bertolini championed this new vision along with several of the other senior leaders. But, I think the key was that they recognized that issue of trying to do that internally and were willing to form a group to be different. To minimize bureaucracy for this group. And, to leverage their capital and assets to support this group. Not many big companies do this well. My impression is that Aetna is and will continue to be successful here. (Full disclosure – I own a minor number of Aetna shares and have believed this since I bought them about a year ago.)
Of course, in today’s market, there’s an explosion of innovation with questions on the short-term and long-term ROI of many initiatives and start-ups. With that in mind, Dr. Saunders pointed out that they don’t want to own everything. They want to create a plug and play platform of enablement. iTriage is a great example of this where they brought in a mobile technology with 2M downloads in 2011 and now have over 9.5M downloads of the tool (on top of massive increases in functionality and integration). You can download it here – https://itunes.apple.com/app/itriage-health-doctor-symptoms/id304696939?mt=8.
Certainly, one concern others have historically had in this space was how to own solutions and sell them to their peers (competitors). Dr. Saunders talked about their ability to do this with ActiveHealth and a perception that the industry is over that issue as long as Aetna can continue to demonstrate that they are good stewards of the data and are keeping the appropriate firewalls in place.
We wrapped up the conversation talking about the social caregiver and game theory. I think both are important in our mHealth / digital world. With the sandwhich generation, this is increasingly important. That is where Aetna is focusing…enablement of the caregiver for infants and seniors leveraging a social approach. This reminds me of their recent announcement of a pilot with PatientsLikeMe. We also talked about game theory and the role of that in healthcare which is a common theme from my discussion with Keas this morning and a theme from the overall conference.
It should be interesting to watch Dr. Saunders and his team and how Aetna continues to pivot.
Key Topics At #WHCC13 In DC
I’m at the World Healthcare Congress (WHCC13) in Washington DC this week. This has always been one of the top 5 events for me to try to come to every year (admitting that there are a few like TED that I haven’t attended due to budget yet).
It’s interesting how trends start to flow within a conference and how the trends change year to year. This year, the key themes that I continue to hear are (in no order):
- Engagement is critical. Between MD and Patient. Between social network / influencers and member. Between employee and employer.
- We have to get past the barriers to health enablement (i.e., legacy IT systems) and make change happen.
- Game theory can help improve engagement.
- Mobile tools are important.
- Data integration has to happen and employers are doing it themselves.
- Biometrics are critical path.
- We can’t solve healthcare if we don’t solve health. The community. Our food choices. Work / life balance. (I would add sleep and stress.)
- Rapid innovation.
- Reform isn’t going to be easy on the employer or the employee.
But, since Twitter is my new note taker…here’s a few sets of tweets for you.
#WHCC13 Interview: Content + Community + Competition = Keas

I had the opportunity to sit down this morning with Josh Stevens who is the CEO of Keas.
“Keas is the most engaging wellness program in the workplace. Keas promotes healthy behavior and teamwork with interactive media that delivers relevant, individualized content to hundreds of thousands of employees. Keas has a proven track record of supporting corporate HR in increasing retention, productivity, teamwork, collaboration, and competitiveness. By rewarding people for achieving simple exercise and nutrition goals, employee health is improved and overall healthcare costs are decreased.”
He is a passionate believer in using fun and social to drive change in healthcare with a focus initially on wellness and then moving upstream to other challenges like disease management.
As CEO of Keas, the market leader in corporate wellness, Stevens is responsible for leading the development and market adoption of the company’s breakthrough wellness platform and applications.
Stevens has over 20 years of experience in product, sales, marketing, and is a recognized leader in driving high-value product experiences that deliver customer delight and investor’s valuation growth.
Prior to Keas, Stevens was Vice President of e-commerce at YouSendIt, Senior Vice President of strategy and business development at TicketsNow, and General Manager of e-commerce at AOL. Prior to his GM role at AOL, Stevens held a variety of leadership positions in business development, product marketing, product management, and corporate strategy.
Some of you may have seen Keas over the years. They were founded by Adam Bosworth who was responsible for Google Health at one point. They’ve gone through a few evolutions, but it seems like they’ve hit on a working model leveraging several principles that we discussed:
- Being intellectually nimble
- Developing holistic and integrated solutions
- Using content, community, and competition to drive engagement
- Building social networks around health
- Integrating into the consumer’s experience to be seamless (e.g., single sign on)
- Recognizing that change is dependent upon corporate culture changing also
- BYOD (bring your own device) meaning that they can integrate with anyone with an open API
- Realizing that while some people (like me) might want to focus on data in a Quantified Self manner, we’re only 15% of the population
While Josh isn’t a healthcare native, that seems like a good thing. I’ve seen a lot of people try to come into healthcare from the outside. Most of them fail because they get overwhelmed by the regulation or frustrated by the challenges or stick too much to what they personally think should work. In the hour we spent together, I didn’t get that sense.
I’m looking forward to learning more about Keas and trying out the tools myself. One of the most fascinating points was that they get people to engage 15 times per month. I told him that that was a ridiculous number in healthcare. We went on to talk about his hiring a team from the gaming industry and that they were used to being tied to repeat visits not simply getting people to download the tool.
IMHO – if you could get 50% of people to engage twice a month with a tool (and sustain that engagement rate), you would be a hero.
As I’ve talked about in my posts about CVS and as I tweeted earlier today from the conference, companies need to engage the worker at the workplace to transform healthcare. Josh gets that key point.
“Today’s employees spend most of their daily lives at work and companies can have a huge impact on improving overall health by creating a culture of wellness at work. That culture starts with Keas’ fun, engaging platform, which helps employees become healthier, more productive and more engaged at work, and in life.” (press release)

Why CVS Caremark Asking For Your Weight Is Good For You
I continue to annoyed by all the fear-mongering in the industry around what CVS Caremark is “doing to their employees”. What about focusing on how they are helping their employees to get better? (If interested, you should read some of the information they have on their blog.)
Our “Plan for Health” combines an evolving, best-practice approach to health coverage with preventive care and wellness programs. Our colleagues will be more accountable for taking control of their health and associated costs. The first step is getting to know your numbers by getting a health screening and completing an online wellness review each year. If colleagues complete both by the May 1, 2013 deadline, they will avoid paying an additional $600 for the 2013-2014 plan year. (from the CVS Caremark blog)
I was hopeful to hear someone come out strongly and speak about it yesterday on CBS, but instead the CEO of Mercer just talked about “soft” programs that depend upon consumers being proactive around their health. I would rather hear about the value of screenings and how it helps employees. In talking with one friend of mine at a biometrics company, he told me that in one case almost 40% of the people that they identified with diabetes (or pre-diabetes) and hypertension (or pre-hypertension) didn’t know they had the disease (or were at high risk). That to me is a valuable insight to the individual especially when coupled with a program to help them learn and manage their disease (or risk).
For example, companies for years have been using Health Risk Assessments (HRAs) to try to baseline employee health and use that to accomplish several things:
- Help the employee to understand their risks
- Identify people who should be in coaching programs to improve their health
- Learn about their population and how to improve their health benefits
Use of biometrics is the right evolution from the HRA. People have tried HRAs for years with some success. Companies pay as much as $600 for people to take this online survey that has no necessary link to reality. Most HRAs aren’t linked to lab values. Most HRAs aren’t linked to claims data. Most HRAs don’t necessarily trigger enrollment in health programs. They are supposed to activate the employee to be proactive which doesn’t work for many sick consumers especially those in the “pre-disease” phase. (Here’s a good study that does show some increased activation.)
As I mentioned the other day, this use of biometrics and link between incentives and participation (and ultimately outcomes) is normal and will ultimately improve the link between the workplace and the employee around health.
Let’s take a broader look at insurance to help set some context:
- For life insurance, you have to disclose certain data and depending on the policy level you have to do other things like get a physical and have blood work drawn. That effects your costs and their underwriting.
- For car insurance, if you get in accidents, your costs go up. In some case, you can have a monitoring device put on your car to lower your costs. (like getting blood work done)
- For home owners insurance, your costs go up if you live in a flood zone or a earthquake zone. It also goes up if you have lots of claims.
Whether we want to admit it or not, we do determine a lot of our healthcare costs based on decisions we’ve made or had made for us since we were kids. Some of these are conscious and some are subconscious. And, obesity which is a large driver of many of these chronic conditions and has an impact on your likelihood of having cancer. So, a company asking for your BMI and other data to help understand your risks for healthcare costs (of which they typically pick up 80%) doesn’t seem unusual.
Certainly, some are environmental such as those that live in “food deserts” like Detroit. In other cases, workplace stress can affect our health. We’re just starting to get smarter about “sitting disease” and it’s impact on our health. Or, we may take medications that affect our blood pressure (for example). It’s certainly important to understand these in context of your lab values and discuss a holistic strategy for improving your health with your physician and any care management resources which are provided to you (nurse, social worker, nutritionist, pharmacist).
This idea of learning more about employees in terms of biometrics, food, sleep, stress, social interaction, and many other data points is going to be more and more of a focus. Companies want to learn how their employees do things. They want to understand their health. They want to improve their health. They want to invest in their workforce to improve productivity, innovation, and ultimately job satisfaction.
While the glass half-empty people won’t see this and there are some companies that don’t always act this way, I generally believe that companies are trying to act in a way to increase their top line and most intelligent executives understand the correlation between health and wealth and the link between employee satisfaction and growth.
Ultimately, healthcare costs are estimated to put a $240,000 burden on us after we retire (even with Medicare) so if someone wants to help me become healthier and thereby save me money which improves my ability to retire and enjoy life I’m happy for them to do.
Life Through #QuantifiedSelf Glasses
No…this is not about how Google Glass can impact healthcare although I do believe it can and will (something many are talking about).
This is about how the QuantifiedSelf movement can change your view of the world. Ever since I’ve been using the FitBit (see my review) and focusing on getting 10,000 plus steps per day, I’ve noticed a change in how I view the world.
Here’s some examples:
- We got 12″ of snow yesterday. I was immediately thinking about how great of exercise it would be to shovel the snow. I was excited to go out several times and shovel.
- When I was flying today, I was thinking “hopefully we’ll get dropped off at a far gate so I can get in some extra steps.”
- I’ve been excited to clean the house and get in the steps from cleaning.
- I look forward to grocery shopping.
- I park farther away in the parking lot.
- I’m sometimes intentionally less productive at home to get a few extra sets of stairs in for the day.
- When I’m cutting brownies, I’m calculating out how many brownies are supposed to be in the recipe and making sure I cut them to the right size.
- When I eat something, I think about how many steps I’ll have to walk (or run) to burn off that food.
- When I pick meals at a restaurant, I’m always looking for their nutritional menu or going online before ordering.
It’s a totally different way of thinking about life when you look through these “quantified self glasses” to see the world through a “health lense” about calories, exercise, sleep, stress, and other dimensions.
What’s Your #Moment4Change?
I’ve being doing a lot of work lately on how to tackle the obesity problem in the US. This has been great personally as it has forced me to look at lots of research to understand all the tools out there.
- Diet
- Exercise
- Coaching programs
- Devices
- Social networks
- Physicians
- Centers of Excellence
It’s also made me look at different drivers of obesity including sleep and stress. The new report out showing that sitting is a huge problem (even if you exercise) is very eye-opening also.
For years, I’ve talked about my challenges is managing my weight which lead to some fluctuations, but at the end of the day, I think a lot of this boils down to a “Golden Moment” or a “Moment4Change”. Even people who do this every day (e.g., doctors or sports coaches) are often overweight. We have to have something which prompts us to change our life. We aren’t generally motivated by dropping our HDL. We’re motivated by being able to play with our kids or living long enough to see our kids get married.
In my life, there have been several Moment4Change points so I thought I would put this out there to hear what’s motivated others:
- In 2002, I went to the doctor for the first time in a decade. He saw some health risks in my blood work and sent me to another physician. He told me I was obese. (Something less than 50% of physicians actually tell their overweight patients.) I was shocked. I was 215 pounds and 5′-10″. After 2 days of agony, I decided that I couldn’t accept that diagnosis and proceeded to lose 40 pounds in the next 60 days (all through exercise and social motivation through a running group).
- Last fall after letting much of that weight creep back on over the decade, I decided to do a 5K with one of my kids. I’d run 3 marathons and was running several days a week (although at an average pace of 9 minute miles). I got killed as my kid ran at a 7:30 pace in their first race ever. Not only did I feel old, but I felt like I wasn’t being much of a role model. That motivated me to change. Now, after using the FitBit (see several comments), I’ve had good success losing 25 pounds in 3 months and seeing my cholesterol drop 120 points in that same time frame.
So, I’m interested. What has motivated you to changed? And, how do you measure success? I suggested that while women may use the “skinny jeans” test that men might be more likely to use the “belt buckle” test.
RT @gvanantwerp: Is the male equivalent of the #skinnyjeans test the #beltloop test?#quantifiedself #mhealth cc @susannahfox
— healthythinker (@healthythinker) March 14, 2013
I think this image below from the AON Hewitt 2012 Health Care Survey is a good one about the fact that 80% of our costs are driven by 8 behaviors.

I also thought that this presentation at the FMI by The Well which was a GSW project was right in line with this.
A Frustrating Pharmacy Experience Highlights Service Challenges #Fail
We all talk about the challenge of consumer engagement in healthcare. If we can’t get consumers to engage, we’ll never get them to change behavior or be preventative.
But, as the recent Times article highlights, sometimes engagement still leads to failure which can be very frustrating. As I think about my recent experience within the pharmacy system, I’m reminded of a comment that I re-tweeted yesterday.
@reginaherzlinger asks why you need to have connections to get clear information about cost and quality if care.
— Liz Boehm (@LizBoehm) March 16, 2013
In this case, I have connections which I suppose I could escalate this to, but it seems wrong that the only way to resolve my customer service issue is to call in personal favors from Express Scripts and CVS.
@expressscripts #rx #fail. Refill rejected due to @cvs refill I never picked up 3 mo ago. Why is it my issue 2 resolve?Call pharmacy #cx
— George Van Antwerp (@gvanantwerp) March 9, 2013
But, maybe that’s what I’ll have to do. At this point, the only way I seem to be able to get my medication is to pay cash which seems like a total system failure. (Thankfully, I can use the GoodRx app to figure out which pharmacies have the lowest cash price for me.)
So, here’s the scenario…
- On 12/31/12, I requested a refill for my 90-day retail script that was getting filled at my local CVS store.
- I got busy and couldn’t go to pick it up until 1/2/13.
- Obviously, my plan design changed on 1/1/13, and I was no longer eligible for 90-day retail scripts at CVS.
- I asked the pharmacist to run it as a 30-day script. They tried numerous times, but for whatever reason, they couldn’t get the 30-day script to go through.
- I asked them to transfer the script to my local Schnucks (grocery store) pharmacy.
- I filled the January 30-day script and a February 30-day script.
- When I came back for my March refill, they were getting a RTS (refill-too-soon) reject from the PBM – Express Scripts.
- The local pharmacist and I both jumped on our phones and talked to the pharmacy help desk and customer service at Express Scripts and got the same answer…”You should have another 59 days supply based on the 90-day Rx you picked up at CVS on 12/31/12.”
- I tried explaining to the customer service rep that I never picked it up. They said that I’d have to solve that with CVS since they show it in the Express Scripts system…which by the way had me very upset that it became my issue to resolve a problem between the pharmacy and the PBM. The rep went on to explain to me that they don’t talk to retail pharmacies to resolve issues like this. (This became one of very few times when I was shouting and upset on a customer service call.)
- My local pharmacist called the CVS store that said they show the original claim, but it shows that they didn’t fill it. They agreed to try to reverse it again.
- One complicating factor here which I think is making this worse is that the 2012 plan was with Medco which has since been bought by Express Scripts. As a new client to Express Scripts, I would assume Medco sent them an open refill file probably on 12/31/12 or 1/1/13. A reversal after that day might never come over to Express Scripts.
- So, I posted the above tweet out of frustration over a week ago. Express Scripts’ social media team quickly followed-up and assigned someone to work the case…BUT, it’s still not fixed.
- I talked to Express Scripts yesterday, and it was still something they were trying to resolve with CVS.
- I talked with CVS who confirms that they never filled the script and show it never paid by Express Scripts. They blame it on an issue with their software vendor that somehow the reversal was caught in the system. They said it could get resolved in the next 48 hours.
Who knows when this will resolve itself, but everyone seems to be able to blame someone else here. Never mind that the patient (me) can’t get their medication. As someone who tries to look at this from the average consumer’s perspective, this is a nightmare and total customer experience failure. I understand the system. I understand plan design. I know the pharmacists. I know the teams at Express Scripts and CVS. Even with all that, I’m stuck having to go outside the system, pay cash for my prescription, and hope that my paper claim will get processed and hit my deductible in my plan design.
Short Sighted View Of Freedom With NY Soda Ban
There are lots of fundamental issues here:
- Was the law legal?
- Does soda make you fat?
- Should the government be able to steer you to positive choices?
- Did this impact our freedom?
At the end of the day, I look at it very differently. I think the proposed ban was great. I was very annoyed last night to find out it was overturned.
Why?
- I don’t see this as any different than moving unhealthy foods to a less obvious place in the food line at school. It simply was meant to help steer people to make healthier decisions. We should all be thankful for someone helping us since we generally don’t seem to be able to help ourselves.
- Government has to be run like a business. (It usually isn’t.) Obesity is a big driver of costs. It requires more power for public transportation. It requires bigger chairs. It requires bigger hospital beds. It requires bigger ambulances. And, all of us taxpayers pay for this.
- 80% of healthcare costs are driven by personal decisions that we make mostly around diet and exercise. Since most people will end up on Medicare at some point, we need to change the cost curve in healthcare sooner rather than later. Otherwise, we either bankrupt our country or we bankrupt Medicare.
So, enjoy your big 64 oz soda now, but when you’re 69 and Medicare has been rolled back to 70 due to funding challenges, you can smile and remember that you got to enjoy all that sugar for years without anyone trying to help you. (I can picture a great political cartoon here of the patient getting a healthcare bill looking over their shoulder from their wheelchair to see a big pile of soda cups!) Never mind the fact that you’re bankrupt due to your healthcare bills and not able to walk around to keep up with your grandkids.

Source: top-nursing-programs.com
Why It’s So Hard To Improve Consumer Engagement In Healthcare?
I spend a lot of my personal and professional time trying to figure out how to better engage consumers in healthcare. If you can’t engage them, you can’t improve outcomes.
Never mind the fact that people experience about 5,000 messages a day so you have to cut through that clutter.
Even if we do cut through the clutter, people are busy living their lives. They’re worried about their family. They’re worried about the economy. They’re trying to keep food on the table. They are generally overwhelmed with too little sleep and too much stress.
But, let’s even assume that you can cut through the clutter and get them to listen, you still struggle with getting a person at a time when they are open to change. These “golden moments” require them to see value in the change and feel like the short-term effort is worth the long-term gain. This “value exchange” doesn’t often exist. And, with 30% variance in the healthcare system, people often don’t trust the system.
Even with all that in mind, people still don’t engage. They don’t get flu shots. They don’t fill their medications. They don’t understand the messages that are delivered to them.
Here’s a quick image I created for a presentation later this week.
A few of the sources for this are:
- http://nnlm.gov/outreach/consumer/hlthlit.html
- http://www.kff.org/healthpollreport/CurrentEdition/security/upload/8322.pdf
- http://www.businessweek.com/bwdaily/dnflash/content/jun2009/db2009064_666715.htm
- http://www.foxnews.com/health/2013/01/10/flu-outbreak-why-are-so-many-not-getting-vaccinated/
- http://www.cdc.gov/chronicdisease/overview/index.htm
A Compelling Argument As To Why You Need More Germs
“In our modern effort to eradicate disease, we pop antibiotics like candy, apply hand sanitizers with abandon, and gargle mouthwash by the gallon. But this carpet-bombing of germs takes a huge toll on good microbes as well as bad. The March/April issue of The Saturday Evening Post, on newsstands now, reveals recent research pointing to medical problems including asthma, obesity, and chronic sinusitis that might be caused by the absence of certain microbiota in our bodies.” (From a press release about the article Why We Need Germs.)
What if the bacteria in our body was a determining factor in chronic conditions? Would you try to get more bacteria into your body? Would you stop doing things to kill the bacteria? Would this change our eating habits?
This is a fascinating article by The Saturday Evening Post, it shares some research that might explain why two people can have the same food habits and one be skinny and one be fat. (A frustrating thing for many of us.)
You can even learn about a crowdsourcing project that will take your feces and tell you the bacteria in your gut.
In the meantime, you might want to eat more asparagus and garlic. Yummy! And, be less stressed out.
For instance, Bacteroidetes—the microbes linked to slimness—proliferate in the presence of fructans, a form of fructose found in asparagus, artichokes, garlic, and onions, among other foods, notes microbiologist Andrew Gewirtz of Georgia State University. A diet high in fructans might support a good crop of slimming Bacteroidetes. On the other hand, he notes, stress decreases the abundance of Bacteroidetes, suggesting one more way stress causes obesity.
Healthcare Fails Again In Experience Survey
The fact that most people would rate their experience with their health insurer low isn’t a big surprise to most of us in healthcare. But, with the Triple Aim and other quality metrics, the customer experience is becoming an increasingly important metric. Several recent surveys have talked about this as one of the top priorities for hospital systems. And, as use of CAHPS continues to grow, this will be more closely linked with incentives.
“Patient experience is on the radar of hospital executives, especially since Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) scores will soon affect reimbursement,” said Jason Wolf, executive director of the Beryl Institute. “However, the data shows that executives are still grappling with how to implement change within their organizations.” (source)
Like in years past, health insurers just barely nudge out TV service providers to prevent being the bottom of the industry in Bruce Temkin’s Benchmarking work. While I’d love to see healthcare broken out into hospitals, physicians, pharmacies, insurance companies, PBMs, and care management companies, I think we can assume some similar concerns would fall out.
Healthcare companies need to find ways to address this. I think there are several key first steps:
- Defining your customer;
- Mapping their experience;
- Creating personas or segments to think about (i.e., healthy, sick, insured);
- Identifying influences on their experience (some of which you might not control);
- Determining what matters versus doesn’t matter;
- Capturing baseline metrics; and
- Building a continuous improvement process.
A Web Strategy Is NOT A Digital Strategy
I was monitoring a pharma conference over in Europe this morning. I found a few of the dialogues really interesting. One of them was about a company creating all these websites to allow consumers to engage with them. There was then some debate.
It’s not about the channel it’s about the strategy #digpharm
— Samantha Collings (@SamCollings) February 26, 2013
@chrisschulze I agree. Having websites isn’t a digital strategy. That’s a pre-2000 strategy. #digpharm
— George Van Antwerp (@gvanantwerp) February 26, 2013
On the on hand, I can agree that you can do some creative things with the channel, and therefore, I should be too down on someone who is very web centric. (i.e., focus on the strategy) On the other hand, digital is much bigger than web.
I’m sure there’s a lot of views here, but let me share mine in terms of what to consider from a digital strategy:
- A website or series of sites along with a mobile web optimization for devices
- Search engine optimization
- Social (e.g., Facebook, Google+)
- Communities
- Video
- Mobile apps
- Device integration (e.g., BodyMedia)
- Software integration (e.g., EMRs, PHRs)
- Blogging
- Gamification
- Telehealth
- Remote monitoring
- Big Data
- Predictive algorithms
- Location based services (e.g., FourSquare)
- Use of SMS
While there are a lot of complicated images out there trying to show everything around digital strategy, I found this one pretty simple and concise.
Is Healthcare An Investment Or A Cost?
As I’ve been looking at the employer view of healthcare, it strikes me that there are two different fundamental approaches.
- Healthcare expenses are a cost. We want to drive down the costs as much as possible.
- Healthcare is an investment in our human capital. We want to optimize our spend with the best outcomes.
Unfortunately, this likely means that the most vulnerable population is disadvantaged in this model (i.e., the hourly worker who is in a job where they are easily interchanged with another employee).
But, for companies where their biggest asset is their people (e.g., Microsoft), it seems clear that they would want to focus on healthcare as an investment.
This might drive you to make different decisions.
- What if you looked at your formulary (for medications) based on side effects not necessarily costs?
- What if you were willing to pay more for drugs with a clear impact on productivity (e.g., no drowsiness)?
- Would you pay more for facilities that were better able to get people back to work?
- Would you really push people into high deductible plans when this forces them to spend more time figuring out the system and navigating it?
- Would you provide them all with devices to help them manage their healthcare?
- Would you hire health advocates to help them navigate the system?
- Would you provide them all with second opinions for major diseases (e.g., cancer) at no additional out-of-pocket costs?
- Would you make sure to implement a telehealth solution so they weren’t away from the office as much?
- Would you provide them with an onsite gym?
- Would you provide them with healthy food onsite?
It seems like you would look at these types of decisions differently. It wouldn’t be about the lowest healthcare premium. It wouldn’t be about pushing them to a limited network. It wouldn’t be about limiting their choice. It wouldn’t be about shifting costs. It would be about guiding them to make choices that kept them happy, productive, and engaged so that they could do the best work for you.
This would involve addressing stress. It would involve addressing sleep patterns. It would involve helping them create a work-life balance.
Body Peace Treaty As Mentioned On Biggest Loser
I was finally catching up on my Biggest Loser shows yesterday. They talked about the Body Peace Treaty from Seventeen magazine. Not something I read, but there are some good points in the treaty. Here are a few for you.
- Do the little things that will keep my body healthy, like walking instead of hanging on the couch, or drinking water rather than something sugary.
- Appreciate what makes my body different from anyone else’s. I love that I’m unique on the inside, I will try to feel that way about the outside too!
- Support my friends, who just like me, have their own body issues. Hey, we’re all in this together!
- Remember that the sun will still rise tomorrow even if I had one too many slices of pizza or an extra scoop of ice cream tonight.
- Quit judging a person solely by how his or her body looks — even if it seems harmless — because I’d never want anyone to do that to me.
- Remind myself that what you see isn’t always what you get on TV and in ads — it takes a lot of airbrushing, dieting, money, and work to look like that.
- Respect my body by feeding it well, working up a sweat when it needs it, and knowing when to give it a break.
- Realize that the mirror can reflect only what’s on the surface of me, not who I am inside.
- Not let my size define me. It’s far better to focus on how awesome I look in my jeans than the number on the tag.
- Surround myself with positive people. True friends are there to lift me up when I’m feeling low and won’t bring me down with criticism, body bashing, or gossip.
So, while some of the things on the list may be more biased towards young women, the fundamentals are the same for all of us.
10 Lessons Learned From Losing Weight

This is the 3rd time in my life that I’ve lost over 10% of my body weight. I’ve tried it with all exercise. I’ve tried it with all diet changes. And, this time, I think I’ve gotten smarter and am doing it with a combination of both thanks to technology which is helping me to track calories in and out. I try to work towards a 500 calorie deficit every day.
With that in mind, here’s a few lessons learned.
- It doesn’t ever really get easier, but it can become a habit (e.g., running) and the norm (e.g., eating better). It’s a lifestyle not an event.
- You eat more calories than you think. It’s all about Eat This Not That. (e.g., the blueberry bagel I ate the other day had more calories than a Dunkin Donuts donut.) A lot of this happens with bread and rolls and to share a quote I heard the other day – “The whiter the bread, the sooner you’re dead.”
- Food is tied up in all our holidays and celebrations. (e.g., celebrating with cake and ice cream, neighborhood BBQ, holiday dinner) You need to learn to take part in these and then burn some extra calories or enjoy in moderation. You will be very frustrated if everything is about denial and not having access to these foods. As I heard a clinician address this question earlier this week, it’s better to be good 360 days a year than to feel like you’ve failed when you participate in these holiday events.
- Losing weight isn’t just about food and exercise…it’s mental about your attitude. (e.g., do you stress eat and what will you do in the future?)
- It’s worth it, but it’s hard work. I look back at my time doing the Insanity workout and their advertisements. I think they make the point that you have to work hard to get results. (and it’s one of the hardest workouts that I’ve ever tried…and couldn’t finish.)
- You can’t change if everyone around you isn’t changing. Weight is tied into your social circle as many examples have shown.
- It takes a while for people to recognize your weight loss so keep yourself motivated with an end goal. And, make sure to set reasonable goals (e.g., 1-2 lbs a week). Unless you’re on the Biggest Loser and can work out 3 hours+ a day with a controlled diet, you’re not necessarily going to make huge drops each week.
- Technology can help whether it’s BodyMedia, FitBit, Nike Fuel, or one of the many other solutions that are out there. I’d also add both the idea of a device with a tool for tracking calories (food diary).
- Weight loss is tied in with sleep so make sure you get your sleep on a regular basis or you’ll mess up all your efforts.
- Travel with healthy snacks since you’ll end up somewhere hungry and be stuck going to fast food or grabbing the candy bar if you don’t have something with you.

2013 PBMI Presentation On Pharmacy Need To Shift To Value Focus
Today, I’m giving my presentation at the PBMI conference in Las Vegas. This year, I choose to focus on the idea of shifting from fee-for-service to value-based contracting. People talk about this relative to ACOs (Accountable Care Organizations) and PCMHs (Patient Centered Medical Homes) from a provider perspective. There have been several groups such as the Center For Health Value Innovation and others thinking about this for year, but in general, this is mostly a concept. That being said, I think it’s time for the industry to grab the bull by the horns and force change.
If the PBM industry doesn’t disintermediate itself (to be extreme) then someone will come in and do it for them but per an older post, this ability to adapt is key for the industry. While the industry may feel “too big to fail”, I’m not sure I agree. If you listened the to the Walgreens / Boots investor call last week or saw some of things that captive PBMs and other data companies are trying to do, there are lots of bites at the apple. That being said, I’m not selling my PBM stocks yet.
So, today I’m giving the attached presentation to facilitate this discussion. I’ve also pre-scheduled some of my tweets to highlight key points (see summary below).

59% Of MDs Want To Know About Employer Care Mgmt Efforts
I just came across this survey data from January of 2010 where the Midwest Business Group on Health (MBGH) did a survey of physicians. I found it really interesting. Let me pull out a few points with some comments…
- 72% of physicians agree that employers should have a role in improving and maintaining the health of their employees with chronic disease. [Since they ultimately are the one paying the bill, this seems like a reasonable expectation in today’s world.]
- 59% believe that they should be informed about employer efforts to help their patients manage chronic conditions. [This is increasingly becoming important as we move from a Fee-For-Service (FFS) world to a value-based or outcomes-based healthcare environment.]
- 46% agree that employers should have a role in helping employees adhere to their medication and treatment regimes. [Since MDs generally don’t view this as their task, if it’s not someone acting on behalf of the employer, I wonder who they think should be doing this.]
- 32% agree that employers should play no role in the health of patients. [With healthcare impacting productivity and global competitiveness, I think this is an unreasonable expectation.]
- 61% want the employer to provide physicians with information on what is available to patients so they can counsel them on the value of participation. [How would they want this information and what would they do with it?]
- 49% would like to receive workplace clinical screening results to reduce redundancies in testing. [Do the other 51% want duplicative testing?]
- 48% want to receive actionable reports (e.g., screening results, health coaching reports) to support them in treating patients. [I would hope so. If the employer (or really their proxy) is managing the patient in a chronic program, why wouldn’t the physician want this data?]
| The study went on to say that physician’s want employers to provide support around weight loss, smoking cessation, flu shots, and other broad programs. They also want the employer to focus on lifestyle change and health improvement not the chronic disease itself. This makes sense, but in general employees are more focused on trusted information coming from their physician not their employer so there’s a clear gap here. (See graph from Aon Hewitt’s 2011 Health Care Survey, New Paths. New Approaches.)
|
Only 50% Of Healthcare Companies Respond To Twitter Messages – Test Results
12 Of 23 Companies
As I mentioned a few weeks ago (2/2/13), I wanted to test and see if healthcare companies would respond to consumers via Twitter. To test this, I posted a fairly general question or message on Twitter to see the response (see below). Of the 23 companies that I sent a message to, only 12 of them ever responded even after 6 of them received a 2nd message. Those results are shared below. What I also wanted to look at was the average time to respond along with which group was more likely to respond.
- PBMs – All of the 3 PBMs that I reached out to responded. (This could be biased by my involvement in this space since two of them e-mailed me directly once I posted a comment.)
- Pharmacies – Only 2 of the 4 retail pharmacies that I reached out to responded.
- Disease Management Companies – Only 1 of the 3 that I reached out to responded. (I was surprised since Alere often thanks me for RT (re-tweeting) them, but didn’t respond to my inquiry.)
- Managed Care – 5 of the 7 companies that I reached out to responded. (For Kaiser, they responded once I changed from @KPNewscenter to @KPThrive.)
- Health Apps or Devices – Only 1 of the 5 companies that I reached out to responded. (This continues to surprise me. I’ve mentioned @FitBit on my blog and in Twitter numerous times without any response or comment.)
- Pharmaceutical Manufacturers – Only 1 of the 3 companies that I reached out to responded. (This doesn’t surprise me since they are very careful about social media. @SanofiUS seems to be part of the team that has been pushing the envelope, and they were the ones to respond. I thought about Tweeting the brands thinking that those might be monitored more closely, but I didn’t.)
I will admit to being surprised. I’m sure all of these companies monitor social media so I’m not sure what leads to the lack of response. [I guess I could give them the out that I clearly indicated it was a test and provided a link to my blog so they could have chosen not to respond.]
Regardless, I learned several things:
-
Some companies have a different Twitter handle for managing customer service.
- Some companies ask you to e-mail them and provide an e-mail.
- Some companies tell you to DM (direct message) them to start a dialogue.
From a time perspective, I have to give kudos to the Prime Therapeutics team that responded in a record 2 minutes. Otherwise, here’s a breakout of the times by company with clusters in the first day and approximately 2 days later.
| Company |
Response Time (Hrs:Min) |
| Prime Therapeutics |
0:02 |
| Aetna |
1:12 |
| LoseIt |
1:19 |
| Healthways |
2:07 |
| Walmart |
3:01 |
| Express Scripts |
8:35 |
| Kaiser |
29:22 |
| BCBSIL |
47:32 |
| OptumRx |
47:39 |
| BCBSLA |
48:18 |
| Sanofi |
53:30 |
I guess one could ask the question of whether to engage consumers via Twitter or simply use the channel more as a push messaging strategy. The reality is that consumers want to engage where they are, and there are a lot of people using Twitter. While it might not be the best way to have a personal discussion around PHI (Protected Health Information) given HIPAA, it certainly seems like a channel that you want to monitor and respond to. It gives you a way to route people to a particular phone number, e-mail, or support process.
As Dave Chase said in his Forbes article “Patient engagement is the blockbuster drug of the century”, this is critical for healthcare companies to figure out.

The CVS Caremark team told me that they actively monitor these channels and engage with people directly. I also talked with one of the people on the Express Scripts social monitoring team who told me that they primarily use social media to disseminate thought leadership and research, but that they actively try to engage with any member who has an actionable complaint. They want to be where the audience is and to quickly take the discussion offline.
If you want to see the questions I asked along with the responses, I’ve posted them below…







 June 11, 2013
June 11, 2013