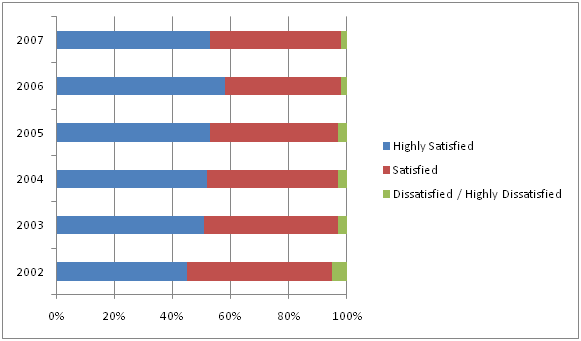
Will incentives be a focus in healthcare? Certainly in lots of other industries, they are a minimum requirement to play at the table – hotels, airlines, banking, consumer products, and casinos. Consumers expect them in many cases. One of the big challenges that any presidential candidate hoping to change healthcare will have to solve is alignment of incentives.
 There is lots of data out there validating this as a focus. In The Road Ahead: Emerging Trends in 2007
There is lots of data out there validating this as a focus. In The Road Ahead: Emerging Trends in 2007
by Hewitt Associates, they say that 48% of employers offer or plan to offer incentives to employees who participate in wellness or health related initiatives. Health plans have started to tier payments based on patient activities around wellness. Companies are paying patients to take HRAs (Health Risk Assessments) and results have shown that the more they pay the better the participation in taking HRAs.
Wellpoint offers employers credits to offset deductibles when members engage in certain activities. Highmark has an outcomes program where members get points for taking classes and participating in other programs. And, IBM offers employees as much as $300 a year for exercising regularly and logging into the companies preventative-care website.
On the other hand, companies like Target have used gift cards as an incentive to get patients to fill their prescriptions at the Target pharmacy for several years. Many companies have used copay waivers or $0 copay programs to encourage patients to try generic drugs. Earlier this year, Democrats in MN recommended giving publicly insured patients $20 gift cards for following their physician’s orders.
patients to try generic drugs. Earlier this year, Democrats in MN recommended giving publicly insured patients $20 gift cards for following their physician’s orders.
Several traditional companies that have worked in other industries are focusing on healthcare. IncentOne is the one that appears to be the market leader with Hallmark Insights and Maritz quickly ramping up.
So, when could you use an incentive:
- If you’re an MCO, you could use incentives for:
- Health Risk Assessments
- Disease Management Program Engagement
- Health Education Class Enrollment
- Brand to Generic Programs
- HEDIS Reminders
- Multi-step Milestone-Oriented Wellness Programs (many employer-group driven)
- Member Portal Registration or Utilization
- Personal Health Record Registration
- Product Design Surveys
- Satisfaction Surveys
- Refer a Friend Programs
- And, if you’re a PBM, you could use incentives for:
- Retail to Mail (or Specialty)
- Retail to Retail (Limited Retail Network)
- Brand to Generic
- Brand to Preferred Brand
- Rx to OTC
- Dose Consolidation Programs
- Pill Splitting
- Cross Sell opportunities with supplies companies—transportation services, DME, etc
- Refer a Friend

 December 10, 2007
December 10, 2007 
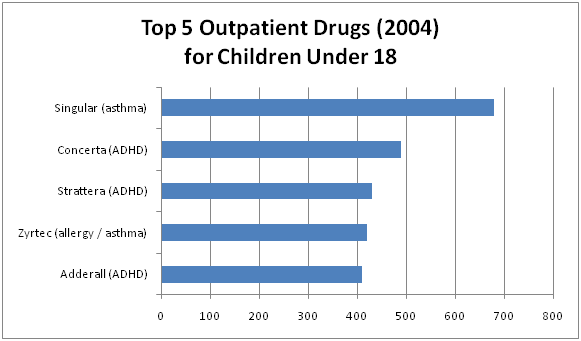
 I had a chance to ride on a plane today with a man who sits on the board of a pharma company. He has worked in pharma for 30 years, and we had a good discussion. One of the things we talked about was the “arms race” in pharma to build up their number of detail representatives. Obviously this changed over the past few years especially with some of the limitations which have been placed on how pharma reps can incent physicians. We went on to talk about the challenge of physicians keeping up with all the drugs on the market and even understanding all the basic
I had a chance to ride on a plane today with a man who sits on the board of a pharma company. He has worked in pharma for 30 years, and we had a good discussion. One of the things we talked about was the “arms race” in pharma to build up their number of detail representatives. Obviously this changed over the past few years especially with some of the limitations which have been placed on how pharma reps can incent physicians. We went on to talk about the challenge of physicians keeping up with all the drugs on the market and even understanding all the basic 




 +
+