I saw this in Drug Benefit News today and thought some of you would be interested. I think Humana’s claims are represented under Argus.
Ingrid Lindberg, Chief Experience Officer, Cigna
This was definitely my favorite and most interesting presentation and discussion from the World Health Care Congress in DC. Ingrid presented and subsequently spent some time talking with me. She has what I would consider one of the coolest jobs – transforming a large company to be consumer centric and radically changing the way they think, speak, and act.
From her presentation, here were a few notes:
- There are 337 languages spoken in the US today. (health literacy issue?)
- Only 23% of people understand what their health insurance policy means.
- Most patients appear to be unaware of their lack of understanding in physician instructions and are inappropriately confident.
- 35% of consumers spend less than 30 minutes reading their health benefit information.
- Only 7% of people trust their insurer.
- Trust translates to loyalty and satisfaction.
- It’s a mix of quantitative and qualitative research.
- They spent time monitoring sites like – www.pissedconsumer.com. (do you?)
- Their senior staff has to spend time listening to member calls each week.
- They spent lots of time on ethographic research and identified 6 personas that they use for defining products – Busy Mom, Skeptic, CareGiver, Controller, Athlete, and Bargain Shopper.
- They identified the #1 dissatisfier was language. Plans talk to them in a language they don’t understand. (For example, consumers think of providers as the insurer not a physician.)
- Consumers didn’t want to be called members since it’s not a health club. They didn’t want anyone other than their physician to call them patient. They’ve elected to go with “customer”.
- She talked a lot about how they’ve changed their EOB (explanation of benefits) and their plan overview to address things like what’s not covered. She talked about how customers think of the EOB as the “this is not a bill form”.
- They identified 10,000 separate letters that could go out to a customer. They’ve re-written 9,000 of them.
- She talked about changing their call centers to 24/7 and the fact that they’ve now taken their 1M call in what used to be considered “after hours”.
- She talked about re-designing their IVR to offer you a self-service option (press 1) or a talk to agent option.
- She talked about their website and YouTube channel – www.ItsTimeToFeelBetter.com.
- She talked about their understanding level being around 70% while the industry average is around 15% [of communications sent out].
- This was in a 15 minute presentation and summarized only 2 years of work.
- She also shared some metrics that they use and improvements such as a 8 point improvement in one year of “values me as a customer”.
And, they’ve shared some of this information in their press kit. There is also an IBM white paper about some of the technology they’ve implemented.
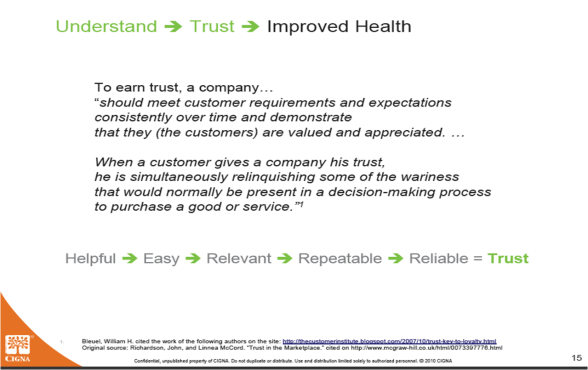
I think the following slide from her deck sums it up well.
Then I sat down with Ingrid to talk with her. I had a thousand questions which I limited to about 10. This is a topic I love and is why I love what I do – work with companies to help them develop consumer communication strategies and implement those strategies to improve the consumer experience and drive better health outcomes.
- How long did it take? This is about a 3-5 year effort which is complicated by the fact that people in these types of roles typically only last about 28 months.
- Did you do it all internally? No. They worked with Peppers & Rogers on a Touchpoint Map and used an IBM tool called Moment of Truth. They also worked with IBM on a new desktop solution. BUT, she was quick to talk about the fact that those were enablers while the majority of work had to be done by internal change agents since this is a cultural change. She said that now almost 80% of Cigna people are using their recommended language and are aware of the changes made by her group.
- Why haven’t others followed? It’s hard work.
- How do you deal with consumer preferences? This is one of my favorite topics to debate. Should you offer consumers options on how you communicate even if you know that they might not pick one that is the most effective. For example, I might say to send me an e-mail, but they get lost, they can’t contain PHI, etc. She said that you have to ask but you have to navigate the path. She seemed to agree with me that there are some communications where you want to ask (e.g., order status at mail) and others where you want the right to contact them (e.g., drug-drug interaction). She talked about the fact that it’s all in the framing (e.g., if we have a message for you that could affect your safety, is it okay if we ignore your do not call request?).
- Are you changing Cigna’s physician communications also? Yes. The changes have become the “language of Cigna”. Physicians are people, and they are also trying to educate physicians on what they’ve learned about how to communicate with customers. She mentioned that the most difficult groups to change were the people that were knee deep in this healthcare language – internal people and consultants.
- Based on my discussion with Andy Webber, I asked her if she thought that today’s fragmented environment would allow for a coordinated consumer experience. She agreed that it’s difficult and that the consumer sees everything as their benefit. They don’t see the piecemeal parts. She mentioned that one of their clients had held a “vendor fair” to kickoff the plan year where she presented their learnings and all the vendors were told to use them immediately. [Maybe that’s part of the solution.]
We then bounced around on a couple of interesting topics:
- We talked about the fact that lots of companies are hiring non-healthcare people to help them better understand the consumer. These include consultants, database people, marketing people, and innovators. My personal opinion is that you need people that have worked in or around healthcare AND outside healthcare. They also need to have consulting and line management experience.
- She talked about their war room (she used another term) where they had a current state and future state (of patient experience) and showed all the 10,000 current communications as a waterfall.
- We talked a little about some of the things we’d done at Express Scripts when I was there including changing the way we referred to members at the call center to patients and the impact that had.
- I shared with her that our biggest difficulty was making web changes at Express Scripts which I thought would be the easiest to do. She shared that changes on the web were one area where they were lagging and is difficult.
- She talked about trying to get innovation from customers by understanding what they want and giving it to them.
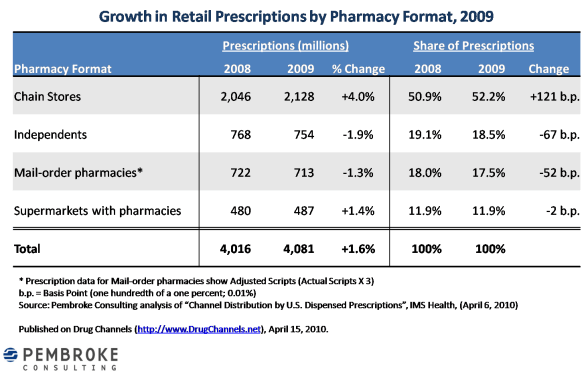
Shifting Marketshare Across Pharmacy Type
Adam Fein just published some analysis showing how marketshare is moving with pharmacies. It shows chains as the only one gaining marketshare.
BOB vs. ERP Concept For Patient Experience
I had a quick dialogue with Andrew Webber (President and CEO of the National Business Coalition on Health) earlier today at the WHCC (see #whcc10 twitter feed). I wanted to talk with him about how we create a unified consumer experience in today’s healthcare environment.
Today, a consumer gets messages from their employer, their physician, their pharmacy, their PBM, their managed care company, their hospital, their disease management company, healthcare sites such as WebMD, and probably several other places. Very little of that is coordinated, and it’s certainly not always consistent in messaging and direction.
Mr. Webber explained that the employers need a “supply chain management” solution to share data across vendors and develop a consistent message. We talked about how the Accountable Care Organization (ACO) concept will try to get us back to some type of solution where there is a primary “owner” of the relationship and that this would be with the trusted key in the solution – the MD.
We talked about the fact that the employers have created this system which pushed the BOB (best-of-breed) over a consolidated, centralized solution. And, we discussed the fact that employers continue to love these “boutique solutions” that develop niche plays (think Health 2.0 companies) which address an acute need. They create great case studies but are often difficult to scale.
It made me think of some old IT models I worked on where clients had to decided whether to pick an ERP system like SAP or go with the best-of-breed and manage the infrastructure to connect them. I think the current employer based system even went a step past this. In the IT world, the company had to manage a connected infrastructure (think enterprise data warehouse and service oriented architecture). BUT, in healthcare (or benefits), that infrastructure doesn’t exist. Each entity owns their piece of it completely with limited interaction and connectivity.
This was the first time where I could see the point of a “employee centric model” versus an “employer centric model”. I’m not sure I believe it could effectively be done, but it reminded me of a company that was trying to create a web-application that was a type of next generation PHR (personal health record) where the member could consolidate communications, designate preferences, and would adapt general (vanilla) communications to the consumer based on behavior, preferences, demographics, etc.
New And Easier Version of Medicare.gov
Got this from CMS…(looks better to me, but it’s been a while since I was there)
Today, the Centers for Medicare & Medicaid Services posted a new and easier to use version of www.medicare.gov, the Medicare consumer-focused Web site. The updated Web site is part of the steps Medicare is taking to make using www.medicare.gov easier for seniors and people who care for them to find the information they need about Medicare. The improved Web site provides users with a summary of Medicare benefits, coverage options, rights and protections, and answers to the most frequently asked questions about Medicare.
The updated Web site reflects Web 2.0 design principles and concepts. The new design was focus tested with seniors, caregivers and operators at Medicare’s helpline, 1-800-MEDICARE, some of the most frequent users of www.medicare.gov. The new design gives Medicare more flexibility to quickly update information that is important to users, especially people with Medicare and family members who care for them.
Take a tour of the new online face of Medicare by clicking on www.medicare.gov.
Accenture Study: Global Perceptions On Health
I’m at the WHCC 2010 in Washington DC, and I got to sit down with Greg Parston from the Institute for Health & Public Service Value from Accenture. They just released the results of their global study – Accenture Citizen Experience Study: Measuring People’s Impressions of Health Care.
How do citizens rate the quality of health care in their countries? How do they view government’s role in supporting – and improving – health and health care? What actions do individuals consider important to making improvements, and how do they rate government’s performance in supporting these actions?
They looked at Australia, Brazil, Canada, France, Germany, Hong Kong, India, Ireland, Italy, Japan, Mexico, Norway, Singapore, Spain, UK, and the US.
Some of the takeaways from the survey:
- People around the world want government to address health disparities – access for people with difficulties and fair and equal access.
- Accountability is a big issue.
- Access to information is essential or very important (although only one of the top three actions for government in India).
- Taking prompt, effective actions to resolve problems or difficulties had the largest gap between expectations and performance…75% rated this as essential or very important with only 26% believing that government performs this well.
But, you can read the study…My value here is the conversation with Greg. Some of the things we discussed were:
- Will the US perceptions and expectations of government shift post-reform? I hope they do the same survey again in a few years for comparitive purposes. In the US, 62% (at time of survey) wanted government to improve healthcare but only 41% trusted the government to do a good job.
- Men have a higher regard for US quality than women. (The US was the only country more focused on cost than quality.)
- The elderly (who have more frequent use) have a higher regard for the quality of the US system than younger people…so, where do the low utilizers form their opinions.
- People feel disengaged and are relatively uninformed in the US. (But, how can this be given all the data that’s out there. And, if the data was available, would people access it and use it?) He believes that people are inquisitive and would use it. The difference between other countries and the US is that there isn’t an integrated system for data. Consumers would have to go to multiple systems to find data. [I’m honestly more of a skeptic here in that the engaged people would soak up more data, BUT the people who drive costs today and in the future (e.g., pre-diabetics) who don’t engage today will still fall thru the cracks.]
- Today, conditional type data (i.e., diabetes 101) is better in the US than abroad, but localized data (MD 1 has better outcomes than MD 2) is worse.
- What would you do if you were the “Chief Experience Officer” at a plan? He talked about focusing on transparency and pushing data out to the members which would build trust and loyalty. [The question is how to value this and whether it’s relevant in a group market versus an individual market.]
- I told him I’d love to see politicians views (or healthcare workers views) versus the general public. He said they’ve done some of that research in other areas and generally the issue is that politicians are looking for the short-term wins while the consumers have longer thresholds than we given them credit for.
- We talked about generation divides on expectations and technology. The example he used was around EMRs where in general 58% of MDs expect to adopt the technology in the next 24 months, but it jumps up to 80% if you exclude the senior MDs that were surveyed. (On the flipside, 65% of patients want MDs to have EMRs.)
- We talked about the value of metrics and scorecards and the need to publish this data. The risk is making sure they stay useful, get used for decision making, and aren’t dropped randomly in the future.
From the US survey:
Sleep, Work Hours, and Career Choices
I know there are limits on how many hours a trucker can drive per day and limits on how many hours an airline pilot can fly per day. I even think there are some limits on hours that a resident can work in a day. These are all within the past decade.
It struck me as interesting earlier today when I thought about the fact that it is the jobs to which we trust our lives and/or have the highest likelihood of harming us where people are most likely to have worked the most hours and slept the least. Given all the research on the impact of sleep on our health and our decision making ability, shouldn’t this be a bigger concern for us?
- People with weapons – police and military – are highly likely to work in stressful positions with long days.
- People in the healthcare field – pharmacists, nurses, physicians – are highly likely to work in stressful positions with long days.
- People who provide transportation – taxi drivers, bus drivers, airline drivers, truckers – are highly likely to work long hours (at least historically). [I assume these may be stressful jobs, but I don’t know.]
I’m sure there are more, but these were the 3 buckets that jumped out at me.
A Few Recent Posts Worth Reading
Trying to keep up with newspapers, magazines, blogs, and everything else can be a fulltime job. So, I took a quick skim of some of the blogs I follow. Here are a few entries worth reading:
- Genetic Test Reduces Hospitalization For Users Of Warfarin
- Copays – When 95% Savings Isn’t Enough
- Chilmark on WebMD’s Social Media Launch
- Health Reform To Squeeze MCO Profits
- Micro-Obstacles to Health and Wellness
- DiabetesMine (always great)
- Pharmacy’s MTM Challenge (one of my favorite bloggers)
- Rating MDs on Cost
- The Power of FREE
- Medicine is Human
There are lots more, but that’s all I have time to share right now.
Why Are Copay Waivers So Popular?
It seems like whenever I talk to companies about adherence one of first things they want to discuss is copay relief. It’s a solution I’ve used before so it’s certainly rationale. But, let’s not forget that cost is not the primary reason for non-adherence. Forgetfulness and lack of health literacy are often big drivers of non-adherence with medications. This is easily validated when comparing lift in medication possession ratio (or more tactically refill rate) by looking at copay waiver type program (value-based design) versus communication programs.
Given that copay waivers often require $10+ per month and other programs can be conducted for much less, I question the ROI. I’d love to see a head-to-head test. Try education and refill reminders versus copay waivers to see which yielded a greater MPR improvement.
My Technology Pulls April Fools On Me
I guess that’s the best way to explain my comedy of issues today.
Issue One: Phone
I was driving from Boston to a meeting in Connecticut. While I hate to drive, I don’t mind it if I can return lots of calls during that time and schedule conference calls during that time. [My first lesson was that early morning in the East Coast is a hard time to call people in other time zones.] About halfway thru my drive, my phone gave me the equivalent of the blue screen of death. It just showed a spinning clock.
So, I pulled the battery out and tried to reset it…over and over again. Nothing. At this point, I’m missing a conference call and thinking about the fact that in today’s day and age no one is going to believe that I was totally off the grid on a day while I’m working. So, 25 minutes later, I pull off the highway to look for a pay phone. (Yes…I’m not even sure they still exist.) I found one and figured I could call someone to send out a message to 4 or 5 people and let them know that my phone was down.
Well, the pay phone didn’t work. So then I spot an AT&T store (which is not my provider). I go in and ask them about a pre-paid phone. They tell me $30 plus pennies per minute. I’m thinking that’s perfect. BUT, the phone comes with no battery life and it’s another $30 for a car charger. No need to be too needy. Fortunately, before I run over my phone with the car, it comes back to life.
Issue Two: Outlook
Even with the delay, I get to my meeting early and decide to stop at a Starbucks and send off a proposal that someone is waiting for. It seems like a great idea, but right after I sit down, I get a call asking where I am. Apparently, I’m still having an Outlook issue with Daylight Savings Time. While I think I’m an hour earlier, I’m actually late (by the time I get back from Starbucks to their office).
Issue Three: Outlook
Now, I get out of the meeting and have too many emails to answer. I scan for a few urgent ones and go to respond. Well, no big surprise…my e-mail is full. I can’t send any e-mails. So, I jump in the car and drive to the airport.
Issue Four: Power
As I look to jump on another conference call, I realize my Bluetooth headset and my phone are low on power. Not a big deal, I just need to find an exit off the highway with some store where I can squat and plug in. Ideally with a wireless network also. I have no idea where I stopped, but I found a Borders which worked. (I’m sure I looked funny with my Bluetooth headset plugged in and in use and trading plugs between my phone and my laptop.)
Issue Five: Wireless
Now, I finally have a chance to get online and save down enough files to send an e-mail. Great…but I can’t connect. Something is wrong with my wireless card (which worked the day before). [I must admit I’m starting to go a little crazy at this point.] So, I call our IT people, but I have to be on conference calls so I can’t take their call and can’t get e-mail. I get enough battery life to make it the rest of the trip and leave for the airport. Once there, I connect with the IT people and fix the wireless card.
Issue Six: Details
This one might simply be called stupidity, but in the rush to get my e-mail downloaded at the airport and find a plug, I looked at the departure time thinking it was the boarding time. So, after moving around some chairs to an abandoned gate with a plug, I hear “last call for George Van Antwerp”.
What a day! I’m glad the 90-minute client meeting was a good one. Now only one more hour before the last leg of my trip…a short flight home from Chicago.
National Stress Awareness Month
April is National Stress Awareness Month. [It seems like there are a lot of these type of month / day “designations” lately.] Here are some statistics from a Fast Company (April 2010) article.
- There are two types of stress – Distress and Eustress. [Eustress – positive stress; Distress – negative stress…oversimplified]
- A study of monkeys showed those suffering from more social stress held more abdominal fat (a precursor of heart disease).
- 3 out of 5 global doctor visits are stress related.
- $22.8B is spent on anxiety-related healthcare each year.
- More than 275,000,000 working days are lost in the US each year due to absenteeism from stress.
- Anxiety and mental-health issues are 5x more common today (2007) among high school and college students than they were at the end of the great depression (1938).
- 2/3rds of spoken curse words are a result of stress.
- 1 in 4 Americans admit to taking a “mental-health day” to cope with stress. The cost to employers is $602 per worker per year.
- 62% of Americans are stressed about work.
- Stress fighting products and services are a $14B business in the US.
Voice Personality Is A Powerful Lever To Motivate Health Behavior
This article appeared in HealthLeaders (3/3/10) by two of my co-workers based on some very interesting work they’ve been doing.
It’s not what you say, but how you say it that matters. The “how” includes a number of specific voice attributes, such as inflection, rate of speech, and intonation—all of which contribute to an overall perceived “voice personality.”
Voice is a powerful lever in the ability to effectively communicate your message to ultimately motivate behavior. Would you be more apt to trust the voice of James Earl Jones or the voice of your local car dealer? How do you perceive these voices overall? Which voice personality most effectively delivers a message? The answers, of course, depend on the listener, what is being communicated, and the behavior you’re trying to motivate.
In healthcare, individuals are educated and supported in the decisions they make about their health through communications. This article highlights a recent study of the impact of voice in healthcare communications and how individuals perceive voice as it relates to health messaging.
Specifically, this research analyzes voice selection for interactive automated calls, an effective outreach channel widely used in healthcare to reach and motivate individuals.
Subjectivity in Voice Selection
If you put a small group of people in a room and ask them to describe the voice they hear, the answers will be wildly different: “This voice sounds too perky.” “That one sounds robotic.” “This voice sounds friendly and cheerful.” Reaching a final conclusion about which voice is “best” often is a highly subjective process.
While we don’t consciously listen to an individual’s voice attributes, we do subconsciously assess the voice’s characteristics and create inferences about the speaker. Over the telephone or on the radio, when voice is the focus, we paint a picture of how someone looks, what kind of person they are, their age, gender, and generally whether or not you trust them.
We’re sometimes surprised in the end at how different the person is when we meet him or her face-to-face. By itself, voice impacts our perceptions, which affect how well we understand a particular message.
In healthcare, it is a common belief that people prefer a female voice when receiving messages about their health. Perhaps this is because female voices are perceived as more nurturing and caring; and women are often the caregivers in the home.
But is a female voice equally effective when communicating to all people, of every age, in every region, and for every type of health related behavior? For instance, is a female voice as effective for people of poor health status hearing a message about an important health screening? What about seniors hearing a reminder to take their cholesterol-lowering medications?
Voice Research
To answer these questions, we created a framework to map specific voice attributes with voice personality. We conducted an attitudinal study to learn how people of different age, gender, and region perceive and respond to different voices. We surveyed 3,000 people across the country, in a statistically representative sample of the commercially insured U.S. population.
Participants heard the same short informational wellness message spoken by several different voices representing a variety of ages, gender, and unique voice characteristics. Survey responders were asked to provide their opinions on the following:
- Is the voice perceived negatively or positively overall?
- Which attributes do people generally use to describe a particular voice? (e.g., rate, volume, and age)
- Is the voice perceived as introverted, extroverted, formal, or conversational?
- Is the voice perceived as coming from someone who is more caring and sincere, or someone who is trying to sell something?
- Do people believe and trust the voice?
The survey results provide a powerful depiction of how different voices are perceived by different segments of a population.
What’s in a Voice?
High trust and care/sincerity ratings are important factors when trying to motivate healthcare behaviors. Medication adherence, for example, is associated with the quality of relationship between the patient and the physician. When people trust the voice they hear, and feel that the person speaking to them is sincere, they are more likely to change their behavior.
There are many interesting attitudinal findings from our study including:
- Both men and women across all age groups preferred a male voice to a female voice overall.
- Voices described as fast paced, young, highly extroverted, perky, and animated rated poorly in the trustworthy and caring categories.
- Voices described as moderately paced, middle-aged, and well-spoken/educated, were rated most trustworthy and caring.
- Seniors (those 65+ years old) aren’t as sensitive to voice age as other groups and don’t perceive older voices as necessarily older sounding. By contrast, younger groups perceive “older” voices more negatively.
- Seniors aren’t as sensitive to the rate of speech as younger populations; therefore, slowing the pace may not be as impactful as was once thought for older populations.
- Younger people (18- to 34-year-olds) are significantly more sensitive to voice age and rate of speech, which means very careful selection of voices for young audiences is important to drive behavior.,/li>
- Young people showed stronger opinions overall between men and women when rating the voice gender they prefer. In other age groups, there is general agreement on voice gender preferences. Gender selection is therefore a more important factor for the 18-to-34-year-old age group.
The use of voice to motivate health decisions
The results of this study provide us insight into how people of varying gender, age, region, and health status perceive the voices they hear. Our goal is to validate how specific voices can be used as a lever to change behavior.
Voice, like other communications levers, such as messages and timing, can be selected based on the demographics, purpose, tone, and intent of communication, as well as how voice supports brand identity. By validating attitudinal voice responses against behavioral activity, voice can ultimately become a measurable behavioral best practice in healthcare communications.
While the bulk of our experience supports the conventional wisdom that a woman’s voice is more effective for healthcare communications, our voice research suggests that there are opportunities to use a male voice to measurably move health behavior. A recent outreach program to educate individuals about the importance of colorectal cancer screenings supports our attitudinal research.
The outreach asked if the individual had received a screening during the past two years, and if they planned to schedule a consultation with their doctor. The same message was delivered by a male and a female voice. All population segments, including men, women, Caucasians, Hispanics, and Asians, answered the survey at a higher rate when a male voice was used versus when a female voice was used.
Conclusion
By applying science and measurement, we can determine the voice qualities that are the most impactful for a specific health behavior and for a group of people. There are measurable patterns in overall voice preference. Communications programs aimed at driving individual behavior should include voice analysis.
By measuring and understanding perceived voice personality, our research sheds light on an objective way to effectively apply voice in healthcare communications to ultimately impacts behavior change.
Jack Newsom, ScD, is vice president of analytics at Silverlink Communications, and Ryan Robbins is voice production manager at Silverlink Communications.
Are You Pouring On The Pounds?
Now here’s an example of an ad campaign from NY that my change the way you think about soda.
And, from a recent article in Fast Company:
- Drinking one can of soda per day can add as much as 10 pounds to your weight in a single year
- People do not eat less food when the drink more calories…these are just more calories.
- For every glass of sugared beverage consumed per day, the likelihood of a child become obese increases by 60%
“Snickers is a nutritional wonderland compared to a Coke.”
As someone who has evolved from a 12-pack of Mountain Dew per day in college to 7 Diet Cokes per day until a few years ago to 1-2 Cokes per day now, this may finally push me over the edge. [Although I did go to zero per day for a year, and my weight didn’t change at all.]
Healthy Habits In US Aren’t Good
A few stats from the National Health Interview Survey:
- 61% of adults drink alcohol. [Seems low to me…plus I thought some data showed red wine to be good for you]
- Only 31% get enough physical activity
- 40% do no leisure physical activity
- 20% smoke (and 21% are former smokers)
The report has shown no improvement in physical activity since 1997.
The data did show that education makes a difference. More educated people were less likely to be smoking, more active, less likely to be obese, and less likely to have slept 6 hours or less in the past 24 hours. And, it showed that married adults are more likely to have healthier behaviors than people who are divorced, widowed, or separated.
Health Reform And The PBMs
I’ve been getting a lot of questions about how health reform will affect the PBMs. While I will admit that I haven’t had the time to read all the tweaks and nuances of what was passed and realize it may change, my take is as follows:
- Assuming the PBMs stay part of any government type of solution, this will provide new covered lives for them to manage thereby growing business.
- Retail profits for combined entities like CVS Caremark may be negatively affected as cash patients are processed under negotiated contracts, but in so much as they can increase share at their stores, the ability to manage the distribution location (i.e., Maintenance Choice) may negate this.
- Generic biologics will be accelerated which will be a very positive play for the specialty business as generics have been for the PBMs. This will also allow the PBMs to use utilization management tools (e.g., step therapy) and formulary management tools which will drive savings and keep them as an essential entity.
- Financial disclosure may have a slightly negative effect by creating new reporting and auditing burdens and may ultimately affect client savings as deal parity becomes more normal versus allowing firms with better leverage and negotiating power to drive deeper deals. But, most PBMs are providing transparency today at a client level so this isn’t anything dramatically different.
- The focus on preventative services and wellness programs may actually create an expanded role for PBMs to step into the disease management void (which favors CVS Caremark’s model with clinics, retail, and PBM and Medco with their Therapeutic Resource Centers) and provide more services around critical conditions like diabetes and increase the focus on consumer engagement and adherence.
- The reduction in the donut hole and funding by pharma will negatively impact PBMs as it will encourage seniors to stay on brand drugs which are less profitable than generic drugs but it will increase adherence during the donut hole which will alleviate some of this downside.
- Overall, health reform should be a net positive for the PBMs allowing them to continue to be part of the strategy in reducing health care costs.
More thoughts from Adam Fein on his blog.
Diabetes Alert Day
Tomorrow (March 23rd) is Diabetes Alert Day. Here is some information that CMS shared around diabetes.
Medicare provides coverage of the following diabetes-related services for qualified Medicare beneficiaries:
• Diabetes screening tests,
• Diabetes self-management training (DSMT),
• Medical nutrition therapy (MNT),
• Glaucoma screening (e.g. dilated eye exam with an intraocular pressure (IOP) measurement), and
• Diabetes supplies (e.g. glucose monitoring equipment and therapeutic shoes) and other services (e.g. foot care).
What Can You Do?
As a trusted source of health care information, your patients rely on your recommendations. CMS requests your help to ensure that all of your eligible patients take advantage of diabetes-related preventive services covered by Medicare.
For More Information
The Medicare Learning Network® (MLN) has developed several educational products related to diabetes-related preventive services covered by Medicare:
o The Guide to Medicare Preventive Services for Physicians, Providers, Suppliers, and Other Health Care Professionals ~ this comprehensive resource provides coverage and coding information on the array of preventive services and screenings that Medicare covers, including diabetes-related services.
o The MLN Preventive Services Educational Products Web Page ~ This website provides descriptions and ordering information for MLN preventive services educational products and resources, including diabetes-related services.
o Quick Reference Information: Medicare Preventive Services ~ this chart provides coverage and coding information on Medicare-covered preventive services, including diabetes-related services.
o Diabetes-Related Services Brochure ~ This brochure provides an overview of Medicare’s coverage of diabetes screening tests, diabetes self-management training, medical nutrition therapy, and supplies and other services for Medicare beneficiaries with diabetes.
o Glaucoma Screening Brochure ~ This brochure provides an overview of Medicare’s coverage of glaucoma screening tests, including the dilated eye exam with an IOP measurement.
To order hardcopies of available Medicare Preventive Services products, including the brochures mentioned above, click on “MLN Product Ordering” in the “Related Links Inside CMS” section of the MLN Preventive Services Educational Products Web Page listed above.
Additional Resources
• National Diabetes Education Program (NDEP) ~ This website offers numerous resources to help your patients delay or prevent the development of type 2 diabetes, as well as resources to help your patients manage diabetes to prevent serious complications. Check out “Your GAME PLAN to Prevent Type 2 Diabetes: Information for Patients,” a 3-page booklet to help people assess their risk for developing diabetes and take steps to prevent diabetes. For patients with diabetes, “The Power to Control Diabetes is in Your Hands”, contains information about diabetes and related Medicare benefits.
• DiabetesAtWork.org ~ This website contains information for employers to help them reduce health care costs and improve productivity by keeping employees healthy
• American Diabetes Association ~ This website contains a wealth of information about diabetes, treatment, and prevention.
Gender Bias Of Statins
Statins are cholesterol lowering drugs (i.e., Lipitor, Crestor, Zocor). Millions of people take them and they account for about 10% of drug spend.
There is now some discussion of whether they work equally in men and women. I guess genomics would make you believe that it’s unlikely, but I’ve never heard anything about this discussion before the recent article in Time Magazine.
I don’t have the time to read all the research in depth and there appears to still be some debate so let me simply pull a few interesting things from the story:
* There is little evidence that statins prevent heart disease in women.
* There is evidence that women are more likely to experience the serious side effects of statins than men are. Those include memory loss, muscle pain, and diabetes.
* The data suggests that statins can reduce heart-related deaths but not deaths overall.
* For females to prevent one event (e.g., heart attack), 36 women would have to take Crestor for five years (from Jupiter study).
Google Health And SureScripts
I’m just catching up with this announcement from a few weeks ago. Google Health has added Surescripts to their partner list. This is interesting to me on a few fronts.
1 – Can this solve the portability issue? Today, if you change employers, your prescription history gets reset. If your employer changes health plans or PBMs, your prescription history gets reset. While this isn’t always a major issue, that history is important both for a DUR (i.e., drug-drug interaction) perspective but also from a research perspective (e.g., Medication Possession Ratio).
2 – Google is going to message users about potential DUR issues. That is a big value proposition of the PBMs. Given the other threats to their business model ($4 generics, direct-to-consumer mail order, claims administrators, legislation, pharmacy to employer contracting), is this another issue?
The “Toyota Effect”
While I’m not an expert, all these stories about Toyota get me thinking about prescriptions. Is the rapid acceleration caused by the car or the driver? Is the perception that it could happen contributing to it happening?
From an outside perspective, it seems to be a mix of correlation, causation, and the placebo effect. Here are some definitions from dictionary.com:
Correlation = the degree to which two or more attributes or measurements on the same group of elements show a tendency to vary together.
Placebo Effect = The beneficial effect in a patient following a particular treatment that arises from the patient’s expectations concerning the treatment rather than from the treatment itself.
In the medical world, it’s important to understand the differences between these three. Let’s say you start taking a new medication and feel sick to your stomach. Is it caused by the medication? Does it happen every time you take the medication but not related? Or did you expect to feel sick and therefore do?
People often don’t pause to think about this and test the hypothesis.
[See older post on price and placebo effect.]
Causation = anything that produces an effect.
AHIP On Health Care Reform Legislation
America’s Health Insurance Plans (AHIP) President and CEO Karen Ignagni released the following statement on proposed health care reform legislation:
“For health care reform to work, everyone needs to be covered and the growth in health care costs must be brought under control. Health care reform legislation that does not address underlying medical costs cannot be sustained. Unfortunately, this legislation will drive up health care costs by adding billions in new health care taxes and encouraging people to wait until they are sick before getting insurance.”
Areas of Concern within the Bill
Lack of Cost Containment:
– Does Not Bend the Cost Curve – Health reform legislation that does not address underlying medical costs cannot be sustained. Unfortunately, this legislation lacks a system-wide approach that would actually bend the cost curve downward.
– Pilot Programs – The legislation takes a very timid and limited approach to addressing ways to control costs and improve quality. The legislation needs to take bolder steps by implementing throughout the entire health care system innovative payment and delivery system models that will help move the nation away from reliance on a fee-for-service payment structure and incentivize performance improvement across the board.
– IMAC – The legislation will not provide the comprehensive oversight needed because it would exempt Medicare payments for hospitals, physicians, and other key services from review during the first five years.
– Medical Malpractice Reform – The legislation needs to protect doctors who follow established best practices and implement safe, accountable care models based on the latest scientific evidence.
– Comparative Effectiveness – Comparative effectiveness research needs to look at both the clinical and cost effectiveness of tests, treatments, procedures, and prescription drugs so that patients and their doctors can make the most informed health care decisions.
Premium Tax:
– The legislation imposes a new $70 billion premium tax that the Congressional Budget Office (CBO) has said will be passed on directly to patients. This will raise the cost of coverage for individuals, families, and employers.
Market Reforms:
– Weak Coverage Requirement – The legislation will encourage people to wait to purchase coverage until they are sick, which unfairly penalizes those who currently have coverage. According to CBO, 23 million Americans will remain uninsured once this bill is fully implemented.
– Age Rating – The new age rating requirements will cause premiums to increase for people under the age of 30 by more than 50 percent.
Medicare Advantage:
– Massive Medicare Advantage Cuts – The legislation imposes $200 billion in cuts to Medicare Advantage that will cause massive disruption for the more than 10 million seniors enrolled in the program. If these cuts are enacted, millions of seniors in Medicare Advantage will lose their coverage, and millions more will face higher premiums and reduced benefits.
(See AmericanHealthSolution.org for what AHIP is promoting as a solution.)
Walgreens Continues Acquisitions
I remember probably five years ago observing that Walgreens didn’t typically grow by acquisition. Well, a lot has changed. They’ve continued to grow by acquisition since then recently adding Duane Reade in NY and now USA Drug Stores in Memphis. I keep thinking they’ll either go on the acquisition path around the PBM or divest of their PBM. So far, I’ve been wrong.
With continued rumors of Aetna’s PBM being on the market, Walgreens would seem an unlikely but potential buyer. I suspect that they’re waiting to see if anything ever becomes of the pressure on the CVS Caremark merger and/or whether that can successfully be leveraged to drive significant multiples. I think CVS has shown that the merger can drive retail business especially with their Maintenance Choice offering.
The other question would be who to sell their PBM to, and one has to wonder if the recent reorganization means anything in this area. [Per Dave Snow’s (CEO of Medco) comments, I think they would be the most active potential buyer right now.] All of the non-retail business which previously reported up thru the Walgreens Health Services group is now reporting up thru the retail business. I personally doubt it, but I’ve always been a big believer in the GE model of wanting to be #1 or #2 in a market or trying to clean up my business to sell it.
I personally have always thought a Prime Therapeutics / Walgreens relationship would seem pretty interesting. They both have decent size books of business and together could probably capture lots of efficiencies.
The Stress Of The Healthcare Vote
I don’t spend a lot of time around politicians, but I had the chance this week to spend some time with lobbyists and people working with the lobbyists. One of the interesting things I heard about the healthcare vote is that politicians (especially the Democrats) were unusually stressed out about having to vote.
Basically, they’ve been told that they’ll be blackballed and unable to get any of their own initiatives pushed thru if they don’t vote for the bill.
And, many of them are seeing numbers that show only 50% of their constituents (at best) support the bill.
Therefore, it’s a lose-lose proposition. You’ve been elected to represent the people so you should do what they want. At the same time, we know that consumers are swayed by all the propaganda by both parties and multiple other groups. Do you know better?
It’s a great question. I haven’t been a big supporter of this reform while I 100% agree that our system is messed up. My recommendation continues to be to parse it up. First, solve coverage for the uninsured. Second, begin to address things like previous conditions. Third, focus on prevention and the payment / incentive systems.
And, I’m in the industry and don’t have time to keep up with all the changes and nuances to the legislation. I had finally resolved myself to reform and thought the bill(s) on the table right before the MA vote were probably ok (not great). But, I don’t know what’s changed since then and the meaning of those changes.
I saw some article about all the pork being put back in to the bills to get the vote. That makes me annoyed as a taxpayer.
CVS Caremark Employer Survey
CVS Caremark recently published the results of their 2010 employer survey.
- 94% will seek opportunities to improve savings more WHILE looking for ways to improve the overall member experience
-
They ranked the following as key priorities in their PBM procurement strategy:
- 86% price
- 86% customer service
- 84% trust and reliability
- 46% consumer engagement capabilities
- 48% were considering implementing a step therapy program (generic before a brand)
- 56% were considering a copay waiver to drive adoption of generic drugs
As a consultant and vendor in the consumer engagement space, this is great. Let’s look at these incrementally:
- Price is the standard competitive space. This is already playing out and potentially accelerating with the direct to employer approach of Wal-Mart and Walgreens.
- Customer service is a critical foundation item for both the PBM call center and mail order operations. And, consumer engagement can impact customer service as PBMs learn to predict behavior and proactively engage consumers using segmentation, personalization, and preference-based marketing.
That leaves consumer engagement as a key opportunity for differentiation. And, it plays well to the overall comment about improving savings while improving the member experience. Consumers don’t understand their plan designs. They don’t understand when to act. They don’t understand the importance of adherence.
So, this creates a big opportunity. PBMs can engage consumers to improve 90-day utilization (retail or mail), shift patients to designated pharmacies (retail, mail, specialty), improve generic fill rate (e.g., copay waiver), improve adherence, and allow employers to be more aggressive in their plan design (e.g., step therapy).
In general, the survey was a good reinforcement, but it doesn’t show much in terms of changes in client’s interests. The one thing that did surprise me was that last year 74% said reducing costs was their number one measure of success and this year it was only 66%.
Why Do We Need Healthcare Reform?
This was made a few months ago, but I think it does a good job of addressing some of the core issues.
Insanity Workout
I must admit that I generally go out of my way to not promote products, but I started this new workout routine (Insanity by BeachBody) a few weeks ago and am impressed. Very difficult. I think in the first two weeks that I’ve only made it thru the warm-up twice without stopping. I’ve checked with a few others so I know I’m not crazy. It’s hard.
For me, I needed one that I could travel with (i.e., no equipment needed) and would push me. I’m trying to work on the better eating concept, but that is always my achilles heel.
Light and Sneezing
I’d never heard of this until the other day but apparently 18-35% of the population has something called Photic Sneeze Reflex. A friend first brought this up when she mentioned that she sneezes when going from darkness to light. Apparently, the nerve that controls sneezing is very close to the nerve that controls visual impulses to the brain.
In one story about it, it says it is an inherited trait so kids have a 50/50 chance of having it. Not surprisingly based on when this came up in a meeting this week, some of the people thought this was normal (since they do it) and others thought it was crazy (since they’d never experienced it).
The other thing I learned was that some people with it use bright light to trigger a sneeze which is on the verge but not happening.
12 of Top 50 VC Backed Firms In Healthcare
The Wall Street Journal had a list of the top 50 venture capital backed firms today (3/09/10). 12 of them were from healthcare.
1. Pacific Biosciences
7. Complete Genomics
11. Portola Pharmaceuticals
12. NeuroPace
14. Ventana Health Services
21. Xanodyne Pharmaceuticals
24. Small Bone Innovations
27. Satiety
31. CVRx
33. Oceana Therapeutics
40. PhotoThera
50. Acceleron Pharma

 April 15, 2010
April 15, 2010