Surprisingly, I’ve been happily living in the St. Louis area for almost 20 years. I moved here after going to the University of Michigan for graduate school at Washington University, and I never thought I’d stay. My girlfriend (now wife) moved a year later, and we’ve loved it ever since. We’ve built two houses, had two kids, and made a lot of friends.
I’ve had chances to move many times to Kansas City, San Francisco, Boston, Columbia (SC), Florida, Minneapolis, New York, New Jersey, and several other cities. All of them I have turned down. So, one of the big questions I get asked now days is why are you moving out of St. Louis since you’ve commuted for so long and “enjoyed” it. That’s a tough one, but as someone who cares about my health, let me position this from a health perspective for all of you.
Ultimately, we’re moving for one reason which is to spend more time with my family. Of those 20 years, I estimate that I’ve spent at least 9 of them where I traveled 50-90% of the business days. You can do the math, but if I assume 15 days per month on the road over 9 years, that’s about 1,620 days that I’ve been gone or 4.4 years. That’s a lot of time to miss with your wife and kids.
But, I also see several health reasons for this:
- Most people I know (including myself) sleep better at home and have a more regular routine. No early morning flights. No late night flights. No uncomfortable beds. No loud neighbors. No temptation to work until all hours of the night. And, as I’ve talked about many times, lack of sleep is a major contributor to productivity, decision making, and health.
- You eat better at home and don’t have to eat out every meal which can affect your calorie intake and therefore your weight.
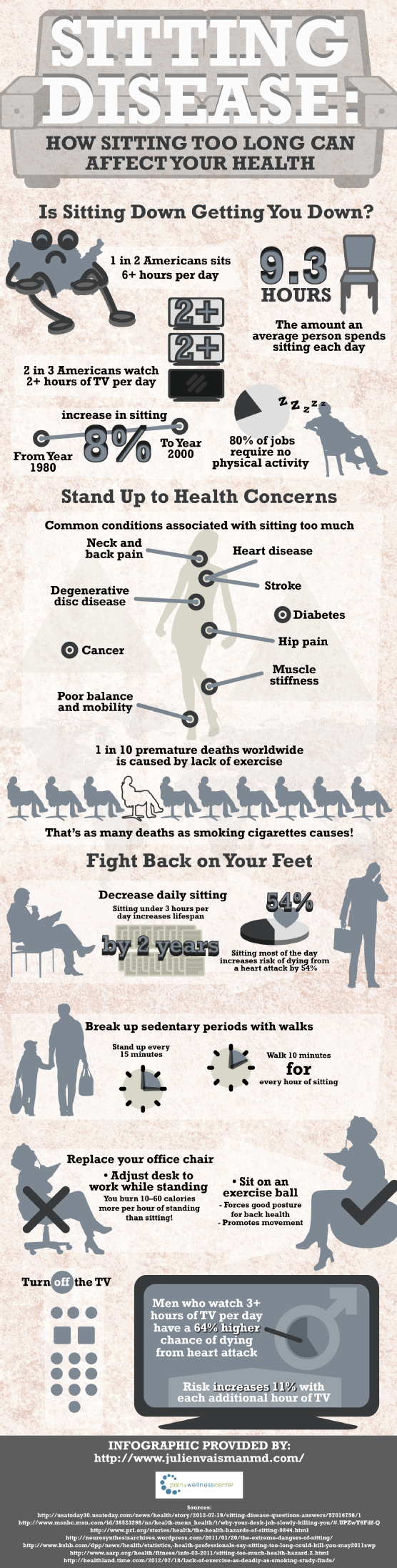
- Long commutes have both mental and physical health implications (none of them good) as you can see in this article and infographic on LifeHacker along with this other article on ABC.
- Being at home and spending time with your family can also affect them (as we know health is social). Here’s one example about eating with your kids that I often quote.
Of course, commuting has some productivity gains (if done right) from a work perspective:
- You can work long days without worrying about other things that you should do when you’re home. (Why do you think consultants are so productive?)
- You can find some nice quiet time on planes to work. (Although this has gone down over time with more crowded flights, more connecting flights, and smaller seats.)
You have to trade this off with productivity lost on travel days (e.g., I wake up every Monday at 4:30, leave for the airport at 5:30, land in Charlotte at 10:15, and get to my office around 11:30 with best case 90 minutes of work done).
But, moving definitely impacts your presenteeism as I’m learning (at least for a few months). After 20 years in one city, there’s a lot to do to move. You have to find new service providers (doctors, dentists, handyman, vet, hair), new schools, new sports teams, new stores, etc.
But, for those of you that aren’t convinced since you think travel is glamorous, let me share just a few stories with you.
- On one of my toughest travel days, I had breakfast with a CIO in Boston at 6:30 am; caught a flight to Minneapolis to give a presentation over lunch; then caught a flight to have a dinner meeting in San Francisco. Long day.
- In some weeks, I used to spend over 20 hours a week in a plane (not including airport time). Talk about sitting disease.
- Just yesterday, when I tried to squeeze in one last trip before I moved, I got up at 3:30 to catch a 6:00 flight. I flew to Florida took a few calls, had a meeting, and then came back to the airport to catch an 8:oo PM flight home. That flight was delayed until 2:05 AM meaning that if I hadn’t just gone to get a hotel room (without any clothes or toiletries) that I would have gotten home 24 hours after I left the house.
Of course, the frequent flyer miles and hotel points are great. We’ve taken many a trip with it. I’ve given my parents free flights. Heck, we’ve even given our dog walkers free flights.
The key is to evaluate several factors which are what I’ve looked at:
- Will you be traveling from which ever city you live in? Don’t move your family just to be traveling out of a new city.
- Do you like the new city and would you consider living there long-term? For example, I know I probably would never like true city living in NY.
- What is important to your family and is it present in the new city? This is a complicated one to find the right mix of services and education.
- Can you afford to live in the new location without a major impact on your quality of life (or will your job account for this)?
Anyways, this has been one reason why I haven’t been blogging as much lately. The move is all consuming especially with lots of things going on at work. I have 4 more days in St. Louis before moving so we’re excited and nervous.

 July 30, 2013
July 30, 2013