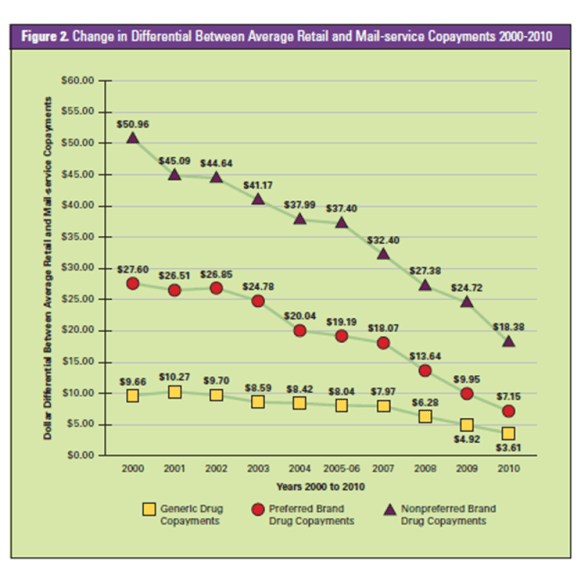
One of the questions I often get is why don’t consumers move to mail as much as they used to. There are several reasons why, but I think this chart from the PBMI 2010-2011 Prescription Drug Benefit Cost and Plan Design Report does a good job of summarizing one issue – less savings. This shows how the savings of moving from retail to mail has gone down over the past 10 years.
Engaging The Distracted Consumer
It’s not a surprise to any of us that most people are much more distracted today then they were in the past. Remember the days when there were no mobile phone, no video games, no DVDs in the car…it seems so peaceful. On the flipside, it seems so unproductive. I can’t imagine not multi-tasking.
Ultimately, there are three questions that come to mind:
- Do we learn more this way?
- Does this affect our social relationships?
- Does this change our productivity keeping in mind quality?
I don’t know the answers to these (although I have opinions). But, I started thinking about this when I was reading an article in Time (Wired For Distraction). The author talks about “continuous partial attention” which is a key complication in the world of health engagement.
On the one hand, I can’t tell you how many times I hear people say how critical multi-tasking is. BUT, there are times (IMHO) that you have to buckle down and focus. I remember a few years ago when I had to essentially just focus on one big project for a month. It was hard, but the project was successful. At the end of the day, there is a difference between being used to distractions and dealing with multi-tasking.

Is this a prevalent issue? Yes. You don’t have to look any farther than those advertisements on TV with the father walking around the soccer field on his BlackBerry or phone. Or look at all the efforts to get people to stop texting while they drive.
“Constant distraction affects not only how well kids learn but also how their brains absorb new information.” (Time, 2/22/11, pg. 56)
I think the study mentioned in the article from UCLA in 2006 makes the point:
- Multi-taskers and focused learners deploy different parts of their brain
- Multi-taskers use their striatum which is focused on building procedural memory
- Focused learners use the hippocampus which helps people apply knowledge
So, what do you want for your kids – them to be good at routine tasks or them to be good creative thinkers. Does that play into Michelle Obama’s decision not to let her kids use Facebook?
But, apply this to the healthcare challenges we face…
- Are people using the devices during their physician visit further limiting what they retain?
- When you send someone a direct mail piece, an e-mail, or a phone call about their healthcare, are they really hearing the information? Or are they listening to TV and reading e-mail? Or taking a phone call while watching a soccer game?
Given the health literacy issues we face, this lack of focus when we’re delivering critical information to an overwhelmed patient is a real cause for concern. Maybe there are simple answers:
- Appeal to the basic research on learning which shows that people learn the most when you leverage multiple ways of delivering information – verbal and written; or
- Simplify the message; or
- Leverage plain language; or
- Ask the person to pause to listen to the message; or
- Increase your attempts to change behavior (without annoying the consumer).
We know the message matters, the channel matters, the person or entity delivering the message matters, and now I’m suggesting that the environment in which the information is received matters.
Chocolate Good For Cholesterol?
Just another one of the many confusing messages in healthcare. Is red wine good or bad? Is this drug good for me? How do I weigh the side effects? How much should I work out? Should I stretch before I work out? Is BMI critical if I have muscle mass? Am I genetically doomed? Should I provide feedback on my physician or will I get sued? Do I have to take my drug every day or just most days?

Well, I’m sure in this case moderation is important, BUT Japanese investigators have found that polyphenols in cocoa attach to genes in the liver and intestines which activate the ones that produce good cholesterol (HDL) and help suppress bad cholesterol (LDL).
Great news for those of us that love sweets!
CatalystRx Engaging Patients With Avatars
 Last week, I got to see one of the more interesting presentations I’ve seen in a while. CatalystRx presented on some of the work they are doing with a mobile application to be released later this year. The application uses an avatar (well technically an “embodied conversational agent“) to engage with the consumer. I’m not sure how well that will work with a senior population, but the technology (shown in a video demo) was very cool.
Last week, I got to see one of the more interesting presentations I’ve seen in a while. CatalystRx presented on some of the work they are doing with a mobile application to be released later this year. The application uses an avatar (well technically an “embodied conversational agent“) to engage with the consumer. I’m not sure how well that will work with a senior population, but the technology (shown in a video demo) was very cool.
The application is based on lots of research (and designed by the people who made Happy Feet). For example, they talked about:
-
-
- The importance of finding the right balance between too cartoonish and too human. They referenced some Disney research about size of the eyes versus the size of the head which creates a positive memory trigger due to similarities to baby’s faces.
- Creating a “trusted advisor” for the patient (using David Shore’s book – Trust Crisis in Healthcare).
- The importance of the face and how it shows emotion (both human and avatar).
- How small talk engaged the consumer and builds trust even when it’s an avatar telling first person stories.
-
Some of the research comes from Chris Creed and Russell Beale’s work.
Recent research has suggested that affective embodied agents that can effectively express simulated emotion have the potential to build and maintain long-term relationships with users. We present our experiences in this space and detail the wide array of design and evaluation issues we had to take into consideration when building an affective embodied agent that assists users with improving poor dietary habits. An overview of our experimental progress is also provided.
The application helps patients to:
- Make decisions
- Identify pharmacies
- See prescription history
- Get reminded about refills
- Get information about generics and formulary compliance
- Receive personalized interventions
Obviously, mobile solutions as a way to engage patients using a secure environment for delivering PHI is a holy grail (for those that download and stay engaged). This was an interesting and promising variation on some of the solutions out there. I look forward to learning more and seeing it once it’s fully available.
Dr. Atul Gawande On Using Checklists
Dr. Atul Gawande wrote The Checklist Manifesto. Here’s a video of him on the Colbert Report talking about using lists.
Do you use checklists?
I do. I’m a big believer in the fact that they help you organize your thoughts. I also believe that in today’s day and age with all the information coming at us and the pace of change that you need to use a list to optimize on the best practice. I recently gave my team a checklist of things to do each week. It’s basically what I think about on each Friday to make sure I can wrap up the week and that I’m prepared for the next week.
PCMA Interview – The Core PBM Skill: Adaptability
Last week, I had a chance to talk with Mark Merritt, President of PCMA, over the phone. I reached out to Mark as a follow-up to my whitepaper on the future of the PBM to get his thoughts on where the market was going. It was a great discussion as I appreciate Mark’s perspective. He spends his days working on behalf of PBMs navigating the changing tides of Washington. He also previously worked with the health plans so he has an appreciation for their perspective as well.
My first question to Mark was about how the PBM model will change in the next 5-10 years.
He reinforced for me that the PBM will continue to drive value. While some had forecasted PBMs becoming commoditized 5-6 years ago, they have continued to grow and demonstrate value time after time. But, he admitted that the exact model they hold in the future is unknown. PBMs have focused on affordability and access and with that mantra, they have continuously changed and adjusted. They’ve evolved from claims processes to trend managers. They’ve moved from mail order companies to add specialty pharmacies. They’ve moved from focusing on rebates to focusing on generics. And, at the same time, they’ve launched new technologies such as electronic prescribing and been critical to the Medicare Part D solution.
He went on to talk about how the relationship with payers has evolved and how PBM clients have become more educated about how to partner with the PBM and not simply look at them as a transactional service where the lowest price is all that matters. [I felt like his comments reinforced a lot of my thoughts about how the PBM needs to be more focused on patient engagement and condition management. Drug trend is not the only answer…outcomes matter.]
We then went on to talk about how PBMs are developing a consumer brand.
Mark talked about consumer branding as a company by company decision since there are a variety of factors to consider. [In my experience, some clients don’t want the PBM to be a “brand” in the consumer’s mind.] We talked about how historically pharmacy has been an after-thought to medical, but that specialty drugs may change that paradigm. We also talked about how an increased focus in preventative medicine would push pharmacy to the forefront where prescription drugs are often first-line therapy for most diagnoses.
We also then talked a little about the difference between the claims processing business of the PBM and the mail or specialty pharmacy. Where the PBM has a pharmacy – patient relationship, their “brand” and awareness to the consumer is [and needs to be] different. They have to be able to engage the consumer to provide them with information and help them understand their drugs, their condition, and help them stay adherent. We wrapped up this section talking about how patient engagement improves savings whether it is on generics, mail order, or overall medical costs.
Finally, we discussed Medicaid growth and some of the research that PCMA has been disseminating around the potential savings with more managed Medicaid and greater use of pharmacy management tools.
My Summary
The summary for me was a reinforcement of why the PBMs have survived. They focus on the patient [while making money]. They evolve to the place where the market needs a solution. They leverage technology. They invest in understanding consumer behavior. And, there are enough of them that clients can find a PBM that fits their needs whether it’s claims processing, mail order, trend management, transparency, limited networks, retail connectivity or some other point of differentiation.
Trying to Limit eRx Functionality
When I first worked on electronic prescribing (eRx) back in 2001, there were grandiose expectations for the technology. A decade later, we’re finally starting to see adoption happen with over 20% of new Rxs (NRxs) written electronically according to several people. (see article or go to Surescripts for more data)
The holy grail of this technology is not simply to get a clean prescription sent electronically, but to minimize the more that 40% of NRxs which fall into the exception process for drug-drug interactions, step therapy rejects, or other follow-ups. (see prior post) That doesn’t even take into account the amount of times that cost is an issue for the patient leading to further work effort by the pharmacy and/or patient to get a new prescription. Obviously, cost is one of the issues which is driving the increased abandonment rate at the pharmacy.
Whether or not physicians should or will take on this additional responsibility at the point-of-care (POC) has always been a question…of course CMS incentives help. BUT, I was disappointed to hear from PCMA that some manufacturers are trying to limit the eRx functionality. They don’t want physicians to be able to:
- See lower cost alternatives
- See drug-drug interactions based on the patient’s history
- See lower cost pharmacy alternatives
That seems a little bitter to me. The manufacturers were one of the biggest advocates of the technology early on to the point where they saw lots of opportunities for promoting their brands. Fortunately, the vendors didn’t sell out as a vendor the retail pharmacies use for messaging did years ago. That vendor allowed the manufacturers to buy out a therapeutic class and didn’t allow any plan specific messaging to be delivered to the consumer which was very frustrating.
Genetics 101 Parts 1-4
I found these 4 videos from 23andMe on YouTube, and I thought I would share them. They answer:
- What are genes?
- What are SNPs?
- Where do your genes come from?
- What is a phenotype?
(Community) Pharmacy 101
The NCPA blog talks about educating Congress about their value. They also share their slide deck .
I’m not sure I see how this is community pharmacy specific, but I agree that this is a good educational deck of what pharmacists do (retail, mail, specialty).
- It’s more than counting pills.
- Immunizations.
- Address adherence.
- Educate patients and serve to support patient centered care and address MD shortage.
- Medication management
I was surprised at the low numbers of non-Rx discussions they have per day and the low number of physician discussions. It would be good to benchmark those based on average store volume.
Social Networking For Pharmacists
Drug Store News has partnered up with Skipta to form a pharmacists social networking site. Interesting.
1. Why Skipta versus some other forum? [Personally I prefer less places to log in not another one]
2. Will pharmacists use it? [TBD]
3. Is it good to have a private social networking location? [Probably if used appropriately]
4. Wouldn’t it be great to use this to facilitate pharmacist and MD dialogue on key topics – adherence?
I’m not sure what else to say on this yet. Obviously, pharmacists have the same issues as doctors – do you friend your patients, what liability do you have for what you say in these channels, is it considered medical advice, etc.
Benefits Package Blog Carnival – Call For Submissions
Next week (2/21/11), I’ll be hosting the 6th edition of the Benefits Package Blog Carnival. You can see last week’s edition at BeyondHealthcareReform.com.
If you’re interested in participating, please send your blog post to me at gvanantwerp at mac dot com. I’d appreciate submissions by Friday night (2/18), but I’ll try to include any I receive by Sunday night (2/20). Please include the name of your blog, the link to the blog post, and your name. Think about submissions that are interesting to people in the benefits space especially thoughts about how they can engage their population to more effectively manage their health.
Thanks.
NCPA Twisting Reality Again
I continue to be frustrated by NCPA (National Community Pharmacists Association). While I agree that the pharmacist – patient relationship is important, they continue to blatantly misrepresent the facts to make their point. On Tuesday, they sent a letter to Kathleen Sebelius, Secretary of HHS, stating the following:
While we strongly support your efforts to provide the states with measures to drive pharmaceutical program costs down, we respectfully disagree with the statement that mail order is a potential cost-savings program strategy. Experience has shown that mail order pharmacies almost never deliver the savings they promise and are often ultimately more expensive than community pharmacies. In 2009, retail pharmacies drove a 69% generic dispensing rate (GDR) while the three dispensing services of the largest PBMs – Medco Health Solutions, Inc.; Express Scripts, Inc.; and CVS Caremark – had GDRs under 58% for the exact same time period – leaving potential savings on the table resulting from increased brand usage.
Either they are naïve or they think HHS is. You can’t compare the GDR at retail pharmacies to the GDR at mail order pharmacies without significant adjustment for acute medications and seasonal medications that aren’t appropriate for mail order. Historically, those medications have had higher generic utilization than other conditions (e.g., antibiotics).
On the other hand, maybe they aren’t a history fan. The only independent study that I’ve seen comparing the two channels specifically on this issue was published in 2004 by Harvard in Health Affairs. It looked at claims from 5 PBMs across both channels, made the adjustments, and concluded that while retail had a slightly better GDR than mail, it had a lower generic substitution rate. It also pointed out that the majority of the different was attributed to the statin class which was over-represented in the mail order channel (and at the time was mostly brand prescriptions).
Or, maybe they haven’t looked at the chain GDR versus the independent GDR…In this presentation, you see what I would expect – chain GDR > independent GDR. Combine that with the percentage of scripts dispensed (i.e., weighted average) and the normalized GDR from the Health Affairs study probably would favor PBMs over independents.
Since PBMs make over 50% of their profits on generic at mail, it wouldn’t make sense for them to sub-optimize this area. Given the changes in drug mix over the past 7 years (i.e., more generics), I would hypothesize that if this study were done again you would see mail order matching or exceeding retail GDR especially GDR for independents.
Growing Mail Order Pharmacy Utilization
A common topic which I discuss with PBM clients is how to improve their mail order utilization. Since more than 50% of their profits come from generics at mail order, this is a critical process. And, while the industry average is 13% utilization (on an adjusted script basis), there are many companies (especially outside of the big 3 PBMs – CVS Caremark, Medco, and Express Scripts) that have much lower utilization and therefore huge value in upside.
Today, I got the chance to speak to investors on this topic courtesy of Barclays Capital. I structured the discussion around three topics:
1. Why is mail order important to the PBM?
2. How do you improve mail order utilization?
3. What are the challenges to improving mail order utilization?
Attached are the slides which I used on the call.
Coupons From Manufacturers
I’ve talked about this a few times. It’s an interesting topic. Are coupons for prescriptions a good thing or a bad thing?
Let’s look at a few perspectives and considerations…
Manufacturer:
- Do they improve my marketshare?
- Do they protect my marketshare from new entrants?
- Do they protect my brand versus generic competition?
- Do they improve adherence (as measured by refill rates)?
- Per point of marketshare, is it cheaper to rebate a drug or offer direct-to-consumer coupons?
- Are coupons more effective than samples? (They are clearly less expensive to produce and distribute.)
- I’d be interested in feedback, but I haven’t found any conclusive data. BUT, I think manufacturers are smart marketers. They wouldn’t be doing this if it didn’t work.
Payor:
- Do the coupons support my formulary? (I would generally think no…otherwise why use them.)
- Do the coupons improve adherence? Are they creating waste?
- Are the coupons changing physician or patient behavior? Is this costing me money (e.g., less generic starts)?
- Is this impacting my total drug spend since the consumer is no longer as price sensitive to copay differentials?
- Do claims processing using the coupons still show up in the patient history such that drug-drug interactions and other safety checks can be conducted?
Customer:
- Am I saving money? [Yes]
- Is the coupon easy to use and understand? [I would think generally yes.]
- They should be asking about their total cost of the drug over time since depending on the condition they may be less likely to convert to a lower cost drug (typically generic) when the coupon is no longer offered. Or, switching drugs may require them to visit the physician or have lab work done that will cost them money.
- They should be asking…if others use this coupon, which means that they are filling a more expensive drug, what does that decision cost me (shared cost)?
As far as I know, there are very few limitations on couponing.
- The state of MA doesn’t allow their use at all.
- There are lots of restrictions about their use in Medicare and Medicaid such that those consumers are usually excluded from using the coupons.
This is generally a topic where there is little known about the answers to these questions (as far as I know).
There was an article in last week’s Drug Benefit News about this topic where I was quoted and built upon a few comments I made about Lipitor earlier:
“Payers are concerned that copay cards incent consumers to use higher-cost drugs,” George Van Antwerp, general manager of pharmacy solutions for Silverlink Communications, tells DBN. “The consumer no longer sees the penalty of using a more expensive drug.”
Pfizer, who declined to comment for this article, has given some indication that it will continue the $4 copay card only until November, when a generic version hits the market, but Van Antwerp says he’d be surprised if the company did not extend the offer. “Back when Zocor went generic, Merck actually made the brand drug cheaper than the generic drug,” Van Antwerp recalls. “United and a few other payers ended up putting brand name Zocor into the generic tier on their formulary.”
Paper Prescriptions Helpful – Duh
I love when someone presents a basic idea as some “new” blockbuster idea. I was just looking through a webinar from last week where it addressed a key point which is increased abandonment of prescriptions at the pharmacy. The presentation referred to a study by CVS that showed that abandonment is higher for e-prescriptions than paper prescriptions. I’ve talked about this before. That physical document (paper prescription) serves both as a reminder, but it also provides the patient with information (drug name, dose, etc) which is an important take away from their visit. BUT, this isn’t new. When I worked with the e-prescribing vendors in 2001, they knew this and offered services where a printout was created for the patient while the prescription was sent to the pharmacy.
Then the presentation talked about actually placing “advertisements” on these printouts. Imagine the ability of the manufacturer to directly message the patient at the time of prescribing with messages about “consider my drug”. This seems to defeat many of the value propositions of e-prescribing which are about pushing plan design information to the physician during the encounter with the patient. Not to mention the disruption to me as the prescriber…imagine the following:
- The MD writes for Drug A which is a generic.
- The MD goes to meet with another patient and tells the current patient to pick up a paper prescription at the counter as they pay their copay.
- When the patient gets their paper prescription, they see messaging around a copay coupon for a branded alternative.
- They then ask to see the MD again to discuss alternatives right then.
Is this really just shifting that discussion from happening later to now or will it lead to a spike in this discussion and pushing it to face-to-face versus on the phone?
Do you have the right amount of pixie dust in your customer experience? (Disney Cruise)
I’ve talked before about the great experience I’ve had on the Disney Cruise Line, and Disney is often held out as a model company. Well…I just got back from a Disney Cruise last week, and I was disappointed. BUT, I learned several things about the customer experience.
- A failure at one part of the process can overshadow other successes
- Expectation management is critical
- Front line employees make the difference
- Keep it simple
Situation:
Let’s set the stage correctly. Disney just added a new boat (the Dream) which is 40% larger than the old boats. This was the third sailing (for the general public) although people had been on the ship for about 3 months. We booked late which impacted our choices, but we upgraded to the concierge rooms at the port.
Food As A Failure:
When you think of cruising, you think of food. It’s a big part of the cruising experience. Although the boat was beautiful and we had a lot of fun, the food was a failure. They have two seatings – 6:00 and 8:30. We couldn’t get into the 6:00 seating which meant we were at 8:30 (which is my kid’s bedtime). So, we requested to get moved to the 6:00 seating (which the concierge should have been able to help us with). It never happened. (I personally can’t believe that there was never a table any night for us to eat dinner at the restaurants since some people go to the adult restaurants and several hundred people didn’t make the trip due to cancelled flights.)
At first, we didn’t care. We’ve cruised before, and there is always a buffet to go to for lunch and dinner. Not on this cruise. Ok, we decided we could survive on room service. We tried that the first night from a limited menu, and the food was disgusting. I’d rather eat at the airport food court. Ok…in concierge, you can order from the family restaurants for room service. We did that, but the food took almost 90 minutes to get to us. That defeated the purpose. Then, to top it off, we put out our card for breakfast in the morning on the last day, and no one ever picked up the card.
In the end, the kid’s club was great. Bingo was fun (we won 3 times). The new cabanas and private beach on the Disney island were very relaxing. BUT, each night as we went to wind down and have a meal, things fell apart. I spent more time chasing food and eating junk then I thought possible.
Lesson: The experience is a collective set of activities not just a few. (i.e., focus on the weakest link)
- Think about the doctor’s office. If the office staff doesn’t greet you, your visit satisfaction is impacted. If you’re bill is wrong, your satisfaction is impacted.
- Think about the pharmacy. If you have to wait too long for your medication, your satisfaction is impacted. If you don’t understand the instructions, your satisfaction is impacted. If you can’t figure out how to log into the website to order a refill, your satisfaction is impacted.
Managing Expectations:
This was our fourth cruise with Disney. The first three we stayed in the same room on the concierge level. By now, there were certain things we expected. All of them seemed to change.
- My kids love the Mickey bars (ice cream). They no longer carry them on the boat.
- One of my kids likes the Mickey mac n cheese. They no longer carry it and replaced it with some slimy version of bad mac n cheese. (Disney should just stick with the microwave Kraft version… it would be better.)
- The dining was always a little “fancy” in terms of the options, but it had some appreciation for the simple foods that kids like. That wasn’t true anymore. (Although we never made it to dinner, I looked at the menus.)
- One of my kids is super picky. He always defaulted to peanut butter and jelly if he didn’t like the food. They always carried Crustables (frozen PB&J). They no longer carry them, and when I asked for bread, peanut butter, and jelly, they couldn’t get it right.
- The concierge always was out to surprise you in the past – chocolate covered strawberries in your room one night or we always got a drawing to take home and frame on the last night. They no longer do that. They’ve moved to a lounge where we come to them. They no longer come to you.
Would I have been more satisfied if I knew this up front, I don’t know. But, I know that learning piecemeal all the changes and hearing “no” to all my requests was frustrating. (Most of these are things they could have anticipated by tracking my past cruising experiences and behavior.)
Lesson: It’s important to know market expectations or expectations from prior experiences and manage them appropriately.
- If you’ve been getting an Explanation of Benefits (EOB) for years, you’ve probably figured out some way to read it (since it’s not easy). If it’s going to change dramatically, you may want to help people understand.
- If you’ve been sending people a generic version of a drug that is colored red and you switch manufacturers to have a blue pill, you might want to let them know.
Frontline Employees Are Where The Rubber Hits The Road:
It’s always easy to sit in the ivory tower and plan out how things will happen, but at the end of the day, I think the Disney question about “did anyone make this a magical voyage for you” summarizes it. It’s the people who make a difference. In every previous cruise, I felt like there were people who went out of their way to know who we were or who my kids were and what they liked. They then would bring them their favorite bread (banana bread) or bond with them in the kid’s club. This didn’t happen. There was one guy at Bingo who made some connection with us, but that was it.
I also find it frustrating that they don’t have any “memory” of me from cruise to cruise. I have the same allergies as last time. Why don’t you use a CRM system to remember the basics about me and validate them?
Lesson: Remember to empower and encourage your employees to engage the customer not simply go through the routine of talking to them.
- When the patient comes into the pharmacy, does the pharmacist or pharmacy technician know their name? Do they at least remember them?
- When your call center agents talk to someone on the phone, do they reference the prior conversations? Do they know what the customer was doing on the website 10 minutes ago that prompted them to call?
Keep It Simple:
This issue has been around forever (aka – KISS). They gave me so many examples of over complicating the process. Let’s just stick with the room. My room (one-bedroom suite) had two TVs. First, one wouldn’t work, but after they fixed it, it made a constant buzzing sound. After 3 calls for service and waiting from 9-11 PM, I finally figured out where the wires were and pulled them out of the wall to stop the buzzing so we could sleep. (It turns out it was just the surround sound which needed to be turned off. Never mind the fact that surround sound isn’t necessary on a cruise, or the fact that there was nothing telling me there was a separate system.)
We also had a whirlpool tub which my son loves, BUT after he used it, it kept going. We couldn’t figure out how to turn it off. (It turns out it takes several minutes after you press the button to clean the tubes, BUT no one tells you that.)
Then we had several lamps in the room, but they didn’t have light bulbs for them. (We didn’t need the lamps, but why put lamps in the room if you can’t supply light bulbs.)
We had two bars of soap – one for the shower and one for the sink. Of course, I grab the sink one to use in the shower. Well, guess what…It didn’t have rounded edges so once it dried you could move it. It was “cemented” to the soap dish. Not to mention that the sink design was such that it wasn’t functional. (Who let the designer in here without any practical experience.)
Now, to top it off, the concierge level is in a gated area which I think is unnecessary, BUT the gates didn’t work. ½ the time the gates were propped open or I had to get down on the floor and put my hand thru the iron fence to reach the inside handle and open it.
Lesson: Focus on what matters and doing the simple things right. Don’t over complicate the process if it doesn’t add value.
- How user friendly is your website? I’m sure most people use the pharmacy website for refills and formulary look-up. Are those prominent and easy to navigate.
- When you get information about your benefits, can you navigate it and understand it? What about lab reports?
*******************
My overall impression is that someone messed up. They brought too many new cast members into a situation without enough experience. They tried to reengineer and change too many things. This should have been a great experience. Being the “chief experience officer” for Disney or the Disney Cruises has to be one of those jobs that people strive for, but my impression is that this person (a) doesn’t have kids; (b) probably never cruised with Disney before; and (c) didn’t spend enough time with the repeat cruisers to understand what they like.
I’ll be interested to see if they respond to my comment card from the cruise. I always hate customer satisfaction surveys that no one takes action on. I see from the message boards that I’m not the only one disappointed with the cruise.
If this was my first cruise with them, I would never cruise with them again. Now, I’m struggling with whether to go back to the old boats in the future or risk the new boats again. We originally booked for the inaugural cruise of the next Disney boat in 2012, but then they changed the inaugural cruise (what a jerk move). But, what this taught me is that experience has residual value. I had three good cruises so I’m likely to try them one more time. I hope they get it right.
And, I hope you see how this translates to healthcare. We overcomplicate healthcare. We make process changes all the time. We don’t manage expectations. There is so much to do to improve this. We have to improve the customer experience in order to get them to trust us and improve our ability to influence outcomes.
Will Physicians As We Know Them Disappear?
It’s not new news. Physicians face a lot of pressure – new drugs, new technology, reform, ever demanding patients, lawsuits, lower pay, less time for cognitive services, … The question is whether we’re at a “tipping point”. In an article in HeathLeaders (Jan 2011, pg. 12), Walker Ray, MD who is head of the nonprofit Physician’s Foundation says there’s a “tsunami out there”. More physicians want to leave practice while baby boomers are just hitting their Medicare years and chronic conditions continue to plague us.
A recent survey by the foundation which published the report – Health Reform and the Decline of the Physician Private Practice – found that only 26% of respondents said they would continue practicing the way they are in 3 years. The report talks about them becoming employees, part-time workers, and administrators. Health reform should create lots of government jobs for them.
BUT, the remaining 74% said they would retire, close their practice, or seek non-clinical jobs (on top of the options above). It’s a critical issue.
We had a shortage of pharmacists a few years ago. That has changed dramatically with new schools, more graduates, and technology. I’m interested to see what happens here. Could something simple like tort reform or payment reform change this trend? Could the ACO model take off and improve this?
A “Difficult” Encounter Leads To Worse Outcomes
An interesting study looks at the percentage of “difficult” patients with some reflection on the physician also. The study showed a few interesting things:
- 18% of patients were considered difficult
- Older physicians and those with better communication skills don’t have as many “difficult” patients
- Difficult patients were 2.4x more likely to have worse symptoms two weeks after their visit
So…what is a “difficult” patient. The article describes them as patients who have lots of unexplained physicial symptoms, stress, anxiety, and other complicating factors.
I think this reinforces a lot of what I talk about. You have to go back to the root of the problem (e.g., adherence) – the patient and physician encounter. We have to make this better. Patients have to understand how to leverage their physician. Physicians need to better understand their patient’s and how to engage them.
Once that infrastructure exists, a lot of things can play out after the fact.
Are You A Defeatist, Catastropist, or a Triumphalist?
In a post by Atul Gawande, he talks about “Seeing Spots“. It’s an interesting piece on the generalized reactions to focusing care on those that really drive the costs in our system.
It’s an important issue. If 5% drive 60% of our costs, why wouldn’t you treat them differently. If 1% drives 40% of the costs (or whatever the number is), shouldn’t you be driving out to their house and helping them.
Of course it’s not a scalable model to the entire population, but 50% success with 5% of the population would save us 30% per year (not accounting for regression to the mean). But, it would be meaningful.
So…which are you?
Best Healthcare Companies To Work For
I was reading through the Fortune 100 Best Companies To Work For and pulled out the list of healthcare companies on there. I was surprised there were not more pharma companies. There were lots of hospital systems. There weren’t any insurers or PBMs.
The top companies across all industries were:
- SAS
- Boston Consulting Group
- Wegmans Food Markets
- NetApp
In healthcare, the companies were:
#19 – The Methodist Hospital System
#27 – CHG Healthcare Services
#35 – Genetech
#36 – Southern Ohio Medical Center
#37 – Scripps Health
#42 – Baptist Health South Florida
#47 – Novo Nordisk
#54 – Atlantic Health
#56 – Millennium: The Takeda Oncology Company
#60 – Children’s Healthcare of Atlanata
#61 – Mayo Clinic
#62 – OhioHealth
#68 – Stryker
#75 – Arkansas Children’s Hospital
#80 – St. Jude Children’s Research Hospital
#88 – Meridian Health
#91 – The Everett Clinic
Some of the perks they call out in the list are:
- Paid volunteer time
- On-site conceirge
- 100% coverage for healthcare
- Unpaid sabbaticals
- Paternity leave
- 401K matching
- Pensions
- Training
- On-site childcare
- On-site gyms
- Charitable matching
- Diversity
The “New” Consumer
In the September 2010 issue of Inc. magazine, there was an article called “Decoding the New Consumer”. It is an interview with John Gerzema, who is the Chief Insights Officer for Young & Rubicam. Here’s a few comments from the article which are elaborated on in his new book – Spend Shift: How the Post-Crisis Values Revolution is Changing the Way We Buy, Sell, and Live:
- Large numbers of people say money is no longer as important to them.
- 76% say that the number of possessions they own doesn’t affect how happy they are
- We are moving from mindless to mindful consumption
- 71% of people say they make it a point to buy from companies who have values similar to their own
- More and more consumers are moving from consumption to production (raising chickens, home canning, bartering)
- 64% of people want to do more things and make more things themselves
- Kindness and generosity are qualities customers increasingly demand from business
- Many Americans no longer consider TVs, dishwashers, and air conditioners to be necessities
- Irony isn’t dead…cynicism is dead.
- Microsoft beats out Apple in reputation, leadership, and being the “best brand”…much of that has to do with the philantrophy of Bill Gates
I think this poses lots of interesting questions for healthcare companies. What is your brand? How is it perceived? What are your values? How do people experience those? How do they add value to your company? How does your call center display these qualities? How do your communications? How do you monitor the shifting of these values and expectations over time?
Patient Responsibility in Readmissions
There has been lots of discussion over the past year about readmissions. With healthcare reform, it is estimated that we can save billions over the next 10 years by addressing this problem.
The new regulations will cut federal reimbursements for ALL discharges if hospitals have a greater than expected 30-day readmission rate. In FY 2013, the cut is one percent, but it goes up from there. I think everyone agrees this is a problem. I’m sure some would debate if this is the right metric, but it certainly is a tangible one.
For those of you that don’t know…In 2009, the NEJM published the article that set this in motion but you can see some of the discussions before this in this nice piece by Academy Health.
“Almost one fifth (19.6%) of the 11,855,702 Medicare beneficiaries who had been discharged from a hospital were rehospitalized within 30 days, and 34.0% were rehospitalized within 90 days; 67.1% of patients who had been discharged with medical conditions and 51.5% of those who had been discharged after surgical procedures were rehospitalized or died within the first year after discharge. In the case of 50.2% of the patients who were rehospitalized within 30 days after a medical discharge to the community, there was no bill for a visit to a physician’s office between the time of discharge and rehospitalization. Among patients who were rehospitalized within 30 days after a surgical discharge, 70.5% were rehospitalized for a medical condition. We estimate that about 10% of rehospitalizations were likely to have been planned. The average stay of rehospitalized patients was 0.6 day longer than that of patients in the same diagnosis-related group whose most recent hospitalization had been at least 6 months previously. We estimate that the cost to Medicare of unplanned rehospitalizations in 2004 was $17.4 billion.”
I think the interesting question here is what is the patient’s responsibility post-discharge.
You have several gaping issues:
- Health Literacy: 2/3rds of US adults over 60 have marginal or inadequate literacy skills and in one study, 81% of patients over 60 couldn’t even understand instructions on a prescription bottle. How are they supposed to navigate the system? (see this site for research on health literacy)
- Memory: Most patients forget what their physician or nurse tells them. I’d always heard that patients remember about 10% of what they’re told (see NYTimes article on this), but thanks to @trishatorrey, I found this study that showed that 40-80% of information is forgotten immediately. Now, some of this could be addressed by having companions at the encounter (see 2002 paper on this), but there have to be better ways to address this systemic issue.
I guess I would add these two together to equal understanding. How are patients who can’t read and don’t remember going to be successful at home.
This article suggests 12 ways to address readmissions. Additionally, our Chief Medical Officer at Silverlink Communications, Dr. Jan Berger, shared some of our research and also did a podcast on the topic last year.
We’ve always struggled with home monitoring. We can’t force the patient to take the pill. It’s also possible that they get prescribed a medication that they can’t afford and therefore don’t fill. They might have transportation issues and not be able to get to a pharmacy.
Another issue is access to a primary care physician for follow-up after discharge. One study estimated that one in five Americans had limited or no access to a primary care physician.
I don’t know about you, but these statistics scare me. You have people at high risk who are the primary cost drivers in our healthcare system, and they aren’t necessarily equipped or supported to be successful.
Now, we’re going to put the burden on the hospitals to fix this. I agree that it has to start there. The question I wonder is how do we link the patient to this somehow. Is there a way to make them responsible for avoiding readmissions by following the discharge instructions? Is there a way to incent them to be successful? What would we systemically have to do to enable them to be more accountable?
This will require a major effort to address physician and patient interactions, address the discharge process, create a follow-up process to education and monitor the consumer, and ultimately to create a system that provides the support they need to improve their health.
I think we all want the right thing, but I’m sitting here trying to figure out how it gets done.
FL Pharmacists to Fight Medicaid Mail Order
The Florida Pharmacy Association along with a local pharmacy in Florida have filed suit against the state for allowing Medicaid patients to use mail order. This seems silly to me. The mail order pharmacy ship has sailed a long time ago. Approximately 13% of all prescriptions filled in the US are through mail order.
While I would still disagree if it was mandatory mail, this isn’t. The state is simply giving patients the option to get their drugs through mail order. If the community pharmacies have an issue, they should match the mail order rates and dispense 90-day prescriptions and delivery them to the patient’s house at no cost.
We’re in a budget crisis here as a country. If we can save money in Medicaid and therefore in the state budgets, why wouldn’t we do it?
The lawsuit says that the change –
“at a minimum deprives the patients’ access to a provider having extensive knowledge of their medical conditions and unique clinical problems.”
Really? I’d love to know how many of those Medicaid patients have a long standing relationship with their pharmacist, know them by name, and don’t use multiple pharmacies. Maybe I’m wrong.
It comes down to losing business BUT if the patients are so happy, won’t they stay with their local pharmacy. This is a transient population so it’s always been hard for mail order. It’s not easy to send them refill reminders. There’s not always a consistent address to mail to. Some of that is changing as text messaging becomes more normal as a communication medium, but that’s still a small percentage of companies.
Medical Data From Thomas Goetz
Here is a video of Thomas Goetz (Wired magazine) from TEDMED…
He talks about redesigning medical data and how to present it for people to understand.
He talks about a key notion of helping people see their way to better health.
He talks about the feedback loop of Personalized Data – Relevance – Choices – Options.
He talks about how Captain Crunch can inspire information delivery for prescription drugs.
And, then he shared the Wired article on redesigning information.
Vaccines and Autism…the Long Path Back
The 1998 article that started this all has been retracted. Well, guess what…it’s going to take a long time for that to permeate the thinking of people across the country (world).
A recent poll by Harris Interactive showed several things:
- 69% of those polled had heard the theory about them being linked BUT only 47% knew the Lancet article had been retracted.
- 18% of people think that vaccines cause autism
- 30% are unsure if they do
- 52% don’t believe they do
That 18% represents a lot of children who aren’t getting vaccines.
USA Today had an article about this the other day. They talked about the fact that 40% of parents have delayed or declined shots for their kids. They point to 5 myths:
- Vaccines cause autism
- Too many vaccines overwhelm children’s immune systems
- It’s safe to “space out” vaccines
- Vaccines contain toxic chemicals
- Vaccine preventable diseases arent’ that dangerous
They go on to point out that there is more aluminum in breast milk (10 mg) and milk based formula (30 mg) than all the recommended vaccines combined (4 mg) based on total consumption in the first 6 months of life.
Compliance For Donations?
Would you be more compliance with your medications if you knew that every time you took a pill or refilled that a donation was made in your honor to a certain charity? It’s an interesting hypothesis being put forth in this article – Leveraging Altruism To Improve Compliance… BUT I personally am fairly skeptical.
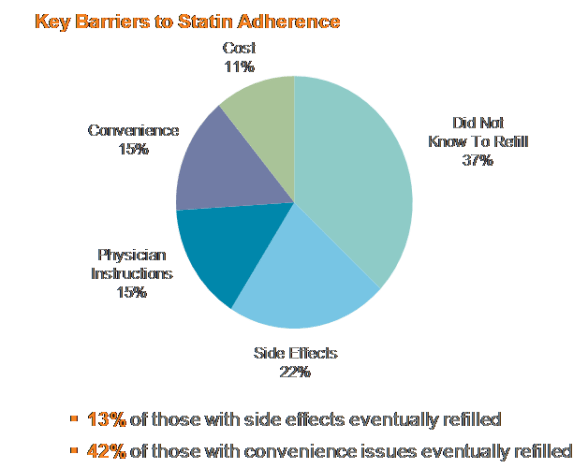
Let’s just look at the barriers identified in one recent barrier survey we did at Silverlink Communications for patients who had not refilled their statin medications.
What do you see?
- Significant literacy issues. People didn’t even know they were supposed to refill.
- People don’t understand the medication and remember what the physician told them.
- Convenience…an easy to address opportunity. These are key targets for a retail-to-mail or 90-day retail program.
- Side effects…this is harder to address but some of it can be managed by setting expectations up front.
Are those going to be addressed because a donation is being made? I don’t think so.
Lipitor Going Generic
If you work in pharmacy, this has been on your radar since Zocor went generic years ago. Lipitor has been the biggest drug worldwide, and I believe the spend in the US is still almost $7B a year even with generic Zocor available. (See Consumer Reports on statins)
Now, it appears that generic Lipitor (atorvastatin) will be available 11/30/11 according to the Pfizer site. It looks like Ranbaxy who was first to file the ANDA will get the 180-day exclusivity (but I know several other generic manufacturers have challenged the patent).
So, what does this mean?
- Lipitor will likely move to the 3rd tier either immediately or at the next formulary update period once the generic is available on the market.
- Atorvastatin will become a part of statin step therapy programs.
- Pharmacies in states that have mandatory generic laws will begin auto-substitution of atorvastatin for Lipitor prescriptions unless there the script has a Dispense As Written (DAW) indication.
- Depending on the pricing of the generic, PBMs and pharmacies will be very aggressive about encouraging use of the generic version (as allowed with the AG settlements from years ago).
We’ve already seen Pfizer take some action which is to promote a $4 copay card (or 30-day sample) for patients. This is to protect market share, but it also makes me wonder if they won’t do something like Merck did by pricing the generic below the Ranbaxy price (see WSJ article).

Given that Pfizer owns a generic company (Greenstone), I have to imagine that they plan to sell atorvastatin thru that company. But, I think the big question that I would be focused on is whether there will be an “authorized generic” (look at the FTC interim report on this topic). This is a big topic in the industry. It allows the manufacturer who owns the patent to allow a generic manufacturer to make and produce a generic version outside of the ANDA process. Right now, it appears that Watson may get to bring an authorized generic of Lipitor to market.
Will you see the same energy around this as you did around Zocor? I remember having a whole “control room” that we developed at Express Scripts to encourage utilization of generic Zocor. It was built around several key things:
-
What were all the channels that a patient communicated with the PBM and how did we educate them around the new generic? [And which could we do at what time so as not to limit the short term rebates that our clients were getting on brand Zocor which kept the prices down until the generic was available?]
- Member portal
- Mail order invoices / stuffers
- Inbound IVR messaging while on hold
- FAQs
- Training call center reps
- Formulary notification programs
-
How did we inform physicians?
- Academic detailing – fax, letter, phone consultations, face-to-face visits
-
What plan design changes did we encourage?
- Step therapy
- What could be done at the POS with the retail pharmacies?
- What could be done at mail?
- How would we track success?
Personally, as a PBM or pharmacy, I’d be trying to lock in a period of exclusivity with Watson or Pfizer to have the limited distribution of the generic Lipitor for a period of time. That would be a huge deal (if it could be pulled off).
Guest Post: The Strong Connection Between Education and Health Outcomes
Is there a correlation between education and health? Studies do in fact indicate that there is a positive relationship between advanced education levels and health outcomes. This association has been well-documented in many countries and for many different metrics of health.
Jobs that require a particular level of education typically provide better access to quality healthcare. Studies indicate that unemployment rates are highest for people without a high school diploma. Additionally, evidence indicates that the unemployed population experiences worse health and higher mortality rates than the employed population.
Other studies have shown that more education can reduce a woman’s risk of depression and obesity. Of course, there are health benefits for men as well: educated men tend to drink less and have less of a chance of dying young.
Multi-Generation Implications
Education has some positive multi-generational implications, as a mother’s level of education is correlated with the health of her children. The parents’ education level affects their kids’ health directly because of resources available to the kids and also indirectly because of the quality of schools their kids attend.
Emotional Health Benefits
Evidence shows that more education means a greater sense of personal control. Individuals who view themselves as having a high degree of personal control report a better health status. These folks are at lower risk for physical ailments and chronic diseases. Also, more education improves an individual’s self-perception of their social status, which also predicts a higher self-reported health status.
Health Literacy
Studies show that only three percent of college graduates have below average health literacy skills. On the other hand, fifteen percent of high school graduates and forty-nine percent of adults who don’t have a high school diploma have health literacy skills that are below average. Reports indicate, not surprisingly, that adults with less than average health literacy are more likely to be considered unhealthy.
Education and Health Report
The authors of the Education and Health Report, David M. Cutler of Harvard University and Adriana Lleras-Muney of Princeton University, find a clear connection between education and health. This connection cannot be completely explained by factors such as the labor market, income, or family background indicators. Health and education have a complicated relationship.
The report shows that for some health outcomes, including obesity and functional limitations, the impact of education appears to be even more positive after people have obtained education beyond a high school diploma. The relationship between health and education seems to be the same for men and women across most outcomes; however, there are a few exceptions.
Race, Education, and Health
Studies show there are few racial differences regarding the impact education has on health. For outcomes that do show differences between Caucasians and Blacks, such as being in fair or poor health, Caucasians tend to experience more positive health benefits from more education when compared to Blacks with the same level of education.
Literacy and Health
Low literacy is associated with adverse health outcomes and negative effects on the health of the population. Additionally, poor literacy skills often contribute to a poor understanding of spoken or written medical advice.
Ten studies showed a positive, significant relationship between literacy level and the participants’ knowledge of the following health issues:
- Contraception
- Smoking
- Hypertension
- Human immunodeficiency virus (HIV)
- Asthma
- Diabetes
- Postoperative care
Clearly, there is a positive connection between education and health. A better educated society leads to better overall health and lower healthcare costs.
Useful Resources
Brian Jenkins writes about a variety of career and college topics for BrainTrack.
Wireless Healthcare Quote
This is from a Qualcomm marketing piece so take it in context, but I thought it was a good quote by Dr. Paul Jacobs (Chairman and CEO):
Consumers have already adopted a wireless lifestyle and the phone in their pocket is not just for voice communications anymore – it’s also becoming the most personal device for information access. Since the mobile phone is always on and always with you, it is the most logical platform for monitoring and maintaining personal health. And new types of mobile devices and services have tremendous potential to improve productivity for medical professionals and help consumers manage their own health. Mobile technology has the potential to improve public health overall and ultimately to make health care more accessible and affordable for all of us.
A Few Health Studies
(Trying to dig out of my work pile and grab a few blog ideas I’ve had on my desk.)
This article in Spirit Magazine (Jan 2011) mentioned 5 different studies that I thought were interesting:
- Too much ice-tea can wreak havoc on your kidneys according to researchers at Loyola University. Add a splash of lemon to inhibit the growth of kidney stones due to the oxalates in iced tea.
- Resveratrol, the anti-aging compound found in red wine, grapes, blueberries, and peanuts, stops out-of-control blood vessel growth in your eyes according to a study by Washington University in St. Louis.
- Women who regularly wear high heels over a 2-year span showed 13% shorter muscle fiberts in their calves BUT a simple calf stretch at the end of the day will keep the muscles in balance according to Manchester Metropolitan University.
- Fast-paced video cames like Call of Duty help players make decisions in other areas of life faster according to researchers from the University of Rochester.
- Researchers at Virginia Tech found that people who drank two glasses of water before a meal lost (on average) 5 pounds more than the non-drinkers during a 12-week study.

 February 25, 2011
February 25, 2011