Last week at the mHealth Summit in DC, I had a chance to sit down and visit with Christine Robins who is the CEO of BodyMedia. (see bio below) One of the most exciting things (mentioned at the end) is their new disposable solution coming out.
Christine Robins is currently the Chief Executive Officer of BodyMedia, Inc., a pioneering market leader in wearable body monitors. BodyMedia’s devices are unparalleled in the marketplace, and equip professionals and consumers with rich information to manage a range of health conditions impacted by lifestyle choices.
Prior to joining BodyMedia, Christine was the CEO of Philips Oral Healthcare where she led the global Sonicare® brand to significant sales and share growth. Christine also has extensive experience in a wide range of marketing and finance capacities gained during her 17 years at S.C. Johnson, where she ran notable brands such as Raid® insecticides, Glade® air fresheners, and Aveeno® skin care. With this background rooted in global multi-national companies and an entrepreneurial zeal essential to lead a high technology upstart, Chris is passionate about developing turnaround strategies, building teams, and driving innovation.
A noted speaker, Christine has delivered presentations at universities such as Harvard, Stanford and Duke, as well as keynotes at industry shows such as the Consumer Electronics Show, Health 2.0 and CTIA. She holds a degree in Marketing and Finance from the University of Wisconsin-Madison and an MBA from Marquette University.
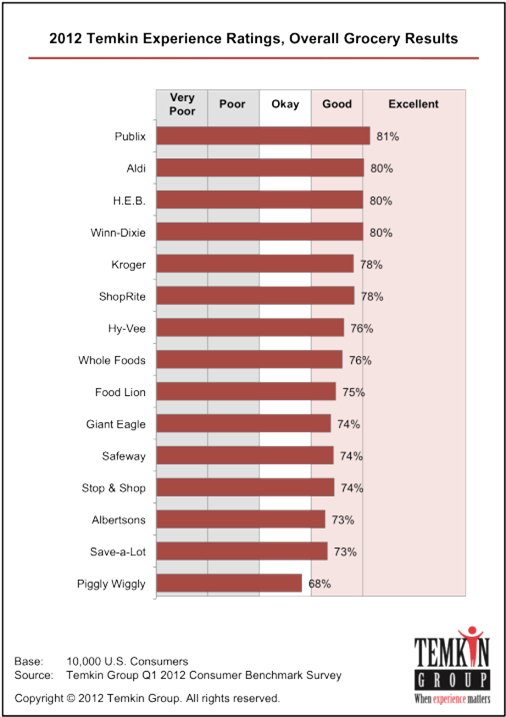
If you’re not familiar with BodyMedia, it’s definitely a company to know from a Quantified Self perspective. They have been around since 1999 providing solutions and have 150 global studies about the effectiveness of their devices in weight loss (see one chart below). The devices that they use continue to get smaller and smaller with time and are registered with the FDA as Class II medical devices.
Their devices track 5,000 data points per minute using 4 different sensors. Here are a few screen shots from the mobile apps that they have.
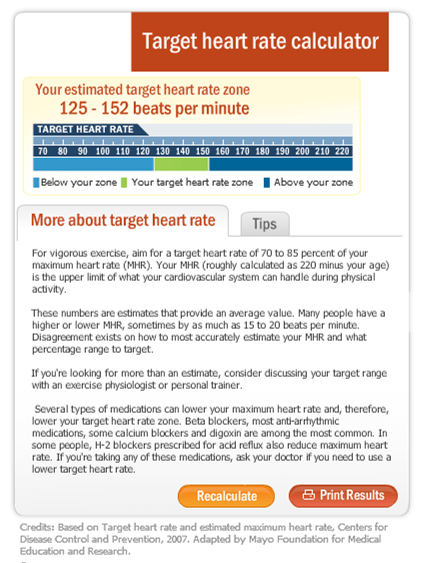
And, as you can see, they map well to the chart below which shows what data consumers and physicians want to track with weight, calories, physical activity, and sleep patterns.
For food tracking, they work with MyFitnessPal which provides them with data on products you eat. I think a good example can be seen in this screen shot from the Android app.
But, honestly, a lot of what I was really intrigued by was a new offering they’re rolling out called the “PATCH” which will be a 7-day, disposable body monitoring system that does everything the full blown system does. I don’t know the price point yet, but this is really exciting as a way to pull new people into the market and to use as a strategy for setting a baseline with a patient to understand their data. It could then lead to recommendations around disease management.
Another thing that Christine talked about was they’re approach to partnering with places like the Biggest Loser and other to allow for a customized content approach to your messaging from the system. She also showed me how the device will project where you will end up at the end of the day based on your past history.
They also have a module for a coach or weight loss professional to help manage and view data across all the people they’re working with.
(And, I just grabbed this image from their website since it points out the 3 key things to weight loss.)


 December 10, 2012
December 10, 2012