I had a chance to sit down and do several interviews at the mHealth Summit earlier this week in DC. I’m slow to get my interviews posted, but they were all very interesting.
One of the best was with Dr. Bettina Experton (see bio below) of Humetrix. I will admit that reading about iBlueButton doesn’t do it justice. I was confused as to what they were trying to do and why it won an award. And, while explanatory after the fact, I found the graphic below intimidating as a consumer before talking with her.

[For those of you that don’t know what BlueButton is, you should go research it here.]
Dr. Experton explained to me how broad the BlueButton initiative now is. I only knew that CMS was using it, but apparently, there are now 200 plans also using it including Aetna, United Healthcare, and Humana. What Humetrix focused on for this offering was the mobile empowerment of BlueButton allowing the patient to have control of their information in the iOS platform (i.e., your Apple products – iPhone, iPad). They provide a tool for downloading and encrypting the data – prescription, medical claims, lab, and procedures.

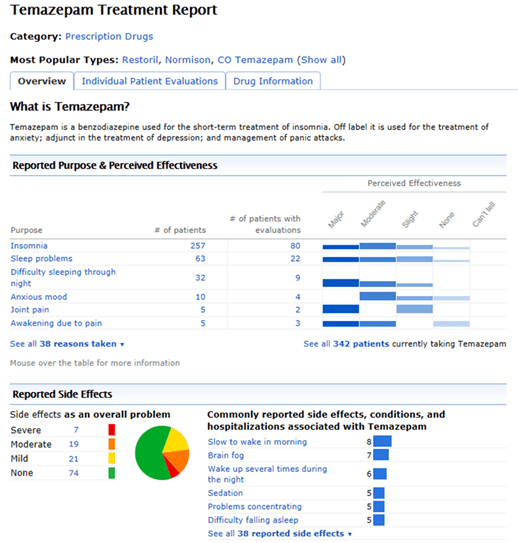
Of course, if you’ve ever seen what this data looks like in the raw form, this wouldn’t seem very helpful. Most of us wouldn’t know what to do with this. But, as Dr. Experton showed me, they’ve rendered the data in a great GUI (graphic user interface) that really brings it to life in a readable and understandable format. For example, they translate the NDC code (used for prescriptions) into the drug name with the chemical name and the dosage. The GUI is very iPod like in terms of simplicity and ease of use.

The iBlueButton app even will pull in patient self-reported data from a PHR (personal health record) and show it in a different color and different section so the provider can understand the sources. Of course, this was another point of confusion for me before we talked which was how would a physician get this and what would they do with it. She showed me a demonstration of the patient opting to share their data and records with the provider in real-time. Of course, this assumes the provider’s office and/or the physician is actually using a device in the presence of the patient, but we know that is changing quickly these days. (See article on survey about MD use of iPad / iPhone.) So, with their tool, I can now store and share my data. The challenge still is integrating this data into the physician’s EMR (electronic medical record), but the iBlueButton app on the provider’s device can do this. It can also print it for those physicians who still want to see the printout in their paper file.
Another thing that you see in the second set of screen shots above is that you can start to report on whether you’re using the prescriptions still that it shows you on. Assuming patients engage, this would be a great tool for medication reconciliation and adherence discussions.
I’m not the Meaningful Use expert, but Dr. Experton pointed out to me that all of this is important since meaningful use requires viewing, downloading, and transmitting capabilities. They provide all of these.
I definitely plan to download iBlueButton and my data, and I hope to use this as a tool to reinforce why any claims provider should be offering you BlueButton access to your data. This is definitely a company to watch.
Bettina Experton, M.D., M.P.H.
President & CEO
Dr. Experton is the founder, President and CEO of Humetrix which she has led over the last 15 years on the HIT innovation path starting with the development of health risk appraisals, chronic care management software, and since the early 2000s with the development of novel mobile device-based solutions which have been deployed worldwide. A physician with over 20 years of healthcare informatics experience, Dr. Experton is the author of multiple information technology patents. At Humetrix, Dr. Experton also conducted groundbreaking health services research on the frail elderly which led to major federal legislation in the area of Medicare and managed care, and has been a national healthcare policy advisor in the US, China, and France. As a healthcare IT advisor to the French Ministry of Health, she made important contributions to the design of the newly launched French government sponsored single web-based individual health record with smart card access made available to French citizens and their physicians. Dr. Experton is an Adjunct Professor of Medicine at the University of California at San Diego, School of Medicine and a permanent member of the Faculty of the School of Medicine in Paris, after graduating Summa Cum Laude where she completed her training in Internal Medicine. In California, Dr. Experton received a Master’s degree in Public Health with a major in epidemiology from Loma Linda University School of Public Health, completed a Pediatrics internship at University of California Davis Medical Center and a Public Health residency with the State of California Department of Health Services.

 March 2, 2013
March 2, 2013