I’ve wanted to try this Xtranormal technology for a while. It was pretty simple. I’m interested in your feedback on whether this is an interesting delivery mechanism, annoying, or fun (see anonymous survey). Here’s the video. [BTW – If you get this in e-mail, you might have to come to the web to view this.]
Seven Million Remote Caregivers (and rising)
In September 2010, Money magazine had an article about the challenges of caring for a parent remotely. For those that do it, the challenge is an obvious one and the toll can be significant. For the rest of us, here’s a few things to understand what they’re going through.
- Long distance caregivers spend an average of $8,700 a year providing support (nearly 2x what those closer spend…largely due to travel costs).
- 49% cut back on leisure activities.
- 47% spend less on vacations.
- 38% have reduced or stopped saving for their future.
- 48% have used sick or vacation hours to care for their loved one.
- 37% have had to either cut back on work hours or quit their job.
- 17% had to take on an additional job or work more hours.
This can be a lot to ask especially for those still caring for young kids at the same time. The article gives a few suggestions:
- Frequent phone check-ins.
- Skype or some other online video chat.
- Local contacts who can help you keep an eye on them.
- Meet their physicians and get a HIPAA consent form signed.
- Look into what help they need – food delivery, transportation, cleaning, paying bills.
- They suggest www.lotsahelpinghands.com for coordination.
- They also suggest PointerWare and InTouchLink for simplifying computer interfaces for the elderly.
- They also suggest contacting the local Agency on Aging.
Healthcare Mash-up Of Articles
Since I’m so far behind, I’m going to share a bunch of things here I think are interesting…
- Prescription Solutions study of compliance within RA…implications for community pharmacy or just a reinforcement of the need for adherence programs?
- Article on predicting persuasion induced behavior change
- Empathy in virtual agents – a change in human interaction
- What do we really know about VBID? – has this died out?
- 5 common diabetes myths – how do we educate people better?
- Gluten: The Whole Story – celiac disease and intolerance to gluten…more people affected than you think
- SwissDent – a toothpaste that uses nanotechnology to oxidize color pigments in teeth (not available in the US)
- Intuitive Eating – eat when hungry
- Technology implications to pharma R&D – EHR data for drug development
- MTM ROI showing 4.73:1 per DBN article (10/8/10)
- 1 in 5 Rxs filled electronically in early 2010
- Working more and not exercising increases a man’s change of heart disease by 50%
CalPERS and Medco
Those of you that follow the industry are certainly aware of this news story. It was definitely a surprise this past week when CalPERS announced that they were dropping Medco as their PBM based on allegations of improper behavior.
For an industry where transparency has replaced years of opaqueness, this will be an issue. Whether Medco is guilty or not-guilty, industry foes will use this to taint the perception of the PBMs. I am sure some people cheered when this came out thinking “finally we may have found something” while the rest of us shook our heads in disbelief.
Happy Fat Holiday!
Not to be a party popper since I love the holidays, and I ate my Corned Beef & Cabbage meal a few days ago (and hope to have another). But, I pulled up a quick recipe to see the calories (700), the calories from fat (470), fat grams, etc. in such a meal (assuming you only eat one serving), and it got me wondering.
If we look at all our holidays – New Years, Valentine’s Day, St. Patrick’s Day, Fat Tuesday, Fourth of July, Easter, Christmas, Thanksgiving, etc., is there any wonder we have food issues? A lot of our favorite memories are tied to holidays which are tied to food. You take those experiences (which typically include some snacks and deserts), and you can eat a few days calories in one day.
Not that it’s bad if you burn off more calories than you take in, but it certainly embeds this food problem right into our culture.
PBMs and Star Ratings
Finally, I’m hearing more talk about PBMs and their role in Star Ratings for Medicare. It seemed like this was a subtlety at the end of last year when I raised it as a 2011 priority.
Drug Benefit News had a story about it in their March 4, 2011 edition with examples from HealthTrans and PerformRx.
In general, there are opportunities to help impact Star Ratings by:
- Blending pharmacy and medical data
- Helping monitor patients on long-term medications
- Increase cholesterol screening
- Increase use of flu shots
- Controlling blood pressure
- Addressing physician communication gaps
- Improving Customer service
- Prior authorization process
- Churn
- Time on hold
- Appeal process
- Accuracy of information provided by customer service
- Managing complaints
- Helping with access issues
- Timely information about the drug plan
- Monitoring use of drugs with a high risk
- Making sure diabetics us hypertension drugs
Since pharmacy is the most used benefit, it can have a very direct impact on the overall satisfaction. It can drive calls. It can be complicated. It can affect perception. And, it can lead to churn.
PBMs need to be working to proactively engage consumers. They need to use data to personalize the experience. They need to use clinical data to identify gaps in care. They need to drive adherence.
I personally hope that the Star “concept” becomes a more normal set of metrics outside of Medicare for measuring success and ultimately leads to a performance-based contracting framework.
Should The State Board Of Pharmacy Govern PBMs?
Mississippi has introduced legislation that would move the oversight of PBMs from the State Insurance Commissioner to the State Board of Pharmacy. From a clinical care perspective, there seems to be some logic here, but from a business perspective, it doesn’t work. Right now, the State Boards are generally made up of local pharmacists with an occassional PBM pharmacist on the board.
Since that group negotiates with the PBMs for rates, it would seem to create a major conflict of interest. PCMA has honed in on this and is actively fighting it.
I guess that’s like saying that hospitals should govern managed care organizations.
Improving Your Call Center Without Just Adding People
In today’s economy, the last thing we want to do is scale up a company by simply adding people. Technology has to play a central role in allowing you to grow your company more efficiently.
At the same time, you want to grow without dropping your level of service. You want to improve the consumer experience.
And, to further complicate matters, you have to manage quality both to make sure that you comply with regulatory oversight and achieve goals around first call resolution. With our rapidly changing healthcare environment and legacy systems in many places, finding, training, and retaining good staff that can continue to keep up with the changes and understand the semantics between plan designs isn’t easy.
So, how do you do that? You’re in a balancing act between cost, quality, and experience.
This is one of the big areas where I’ve seen Silverlink Communications play a role. (Note: There are certainly other efforts which you can undertake in terms of single desktop and process reengineering, but I usually refer in some people I trust for those projects.)
Some people call our technology a “smart dialer”, but there is a difference. If you ever get a call at home from a call center using a dialer, you hear that silence after you say “hello”. The technology is looking for an agent to connect you with. On the flipside, if you’re an agent, you’re being connected with someone or even an answering machine that might not be the right person. That’s what a dialer does.
In our case, Silverlink is using mass personalization, voice detection technology, and speech recognition technology to screen the recipient for the call center. You hear the message right after you pick up the phone. It’s a message that has been carefully crafted using behavioral sciences and health literacy. It asks for you by name and identifies who’s calling for you. It then confirms your identity, and depending on what information is being used in the call, it may have to use multiple forms of authentication to verify who you are. Once we’ve assessed who you are (based on your responses), we’re able to deliver a personalized message to you about your healthcare. That personalized message is scripted in such a way to engage you in a conversation. During that conversation, we can then determine:
- Are you interested in learning more?
- Is this a good time for you to talk?
- Would you like to talk to an agent or hear more now?
- Would you like us to send you information in an e-mail, SMS, or snail mail?
- Would you like a URL to go to for more information?
Occasionally, people ask about authentication. When you send a piece of direct mail, it’s a federal offense to open it if you’re not the intended recipient, but you have no proof that they did that unless your “nanny cam” picks it up. When you call someone, you have a record of when the call was made and what they person who picked up the phone said to authenticate themselves. This certainly seems better to me than any other channel.
Of course, this begs the question of recording all the calls. I’ve heard a few people tell me that they do this with other companies. I find that hard to believe since 12 states have consent laws which would require people to consent to being recorded when they were called. That would limit the effectiveness of the program, or if you didn’t do it, it would open you up to a big lawsuit.
So, how does Silverlink add value to a call center:
- Improving agent productivity. Automating standard questions. Connecting with the right person at the right time.
- Improving consumer engagement. Using behavioral sciences and health literacy to engage people and route them to the right agent based on skill set.
- Improving quality and consistency of experience. Personalizing the experience to engage the consumer but doing it in a way that addresses the clinical guidelines, regulatory requirements, and custom client requests in a consistent manner.
- Improving agent satisfaction. Your agents would rather talk to pre-qualified people or people who have an issue.
- Learning new information. In some cases, patients feel judged when people ask them questions (why aren’t you taking your medications). They may reveal more or other information in an automated environment.
Of course, automated calls aren’t the answer for everyone (although they work better than any other mode other than people…and sometimes beat them also). But, multi-channel coordination is a post for another day.
40% Meat And Wood – Yummy Food
There are numerous strategies for eating better. One simple thing you often hear is to eat simple, natural foods. I think one friend of mine described his diet as the “gorilla diet” (i.e., eat only foods that a gorilla could find naturally).
That being said, I was surprised to hear that something could be considered “beef” even if it only contains 40% beef. This came up in a recent lawsuit where Taco Bell was found to only have 36% “beef” in their products. Does that surprise you?
So, maybe I shouldn’t have been shocked to learn that we are eating wood. Yes. There is wood in some of the food we eat. Well, technically, it’s wood pulp called cellulose that’s used in cat litter, plastic, and food. It gives you fiber and helps canned goods last longer, BUT up to 3.5% of meat can be from cellulose.
These types of stories remind me of when I was in fifth grade eating my hotdog for lunch and found a ziplock bag cooked inside of the hotdog. Sometimes, you don’t want to know what happens in the kitchen / factory. I was glad years ago when I worked on a Y2K project for a big food company that I got the corporate project not the factory project at the meat processing plants.
This information combined with the text message I got from a diabetes program we’re running for a client (as part of the test deployment) which said that you gain 15 pounds a year if you drink a soda a day maybe enough to make me change my eating habits.
Rules Based Communications
After working with data warehouses, configuration engines, and workflow management systems, I’m a big believer in embedding rules into a process. Communications is no different.
Let’s look at a few rules:
- Don’t communicate with someone more than X times per week.
- Don’t call these people.
- Use Spanish for people with that language preference.
- Send a text message to people who have provided their mobile number and opted in to the program.
- When applicable, use a preferred method of communication for reaching out to someone.
- If a caregiver is identified and permission is on file, send the caregiver a copy of all communications to the patient.
- Call the patient if the amount being billed for their prescription is greater than $75.
- For patients between these ages, use the following messaging.
- If the patient hasn’t opened the e-mail after 48 hours, then call them.
- For clinical information, use this channel of communications.
- For John Smith, only call them on Tuesdays between 5-6 pm ET.
- For Medicare recipients, use this font in all letters.
- For Hispanic consumers, use this particular voice in all call programs.
- If the patient doesn’t respond after two attempts, send a fax to their physician.
- For patients with an e-mail on file, send them an e-mail after you leave them a voicemail.
- For patients who are supported by Nurse Smith, only call them when she is on duty and use her name in the caller ID.
I could go on. But, the point is that communications, like healthcare, is a personalized experience. We have to use data to become smarter (historical behavior, segmentation, preferences). We have to use customization to create the right experience. AND, probably the most difficult thing for lots of companies, we have to coordinate communications across modes (i.e., e-mail, direct mail, SMS, automated call, call center, web).
Ultimately, I believe consumers will get to a point where they can help set these rules themselves to create a personalized profile for what they want to know, how they want it delivered, and ultimately provide some perspective on how to frame information to best capture their attention.
To learn more, you should reach out to us at Silverlink Communications.
A Few Allergy Facts
Fortune magazine (7/26/10) had some great allergy data that I thought I would capture here:
- 37M allergy sufferers in the US in 2010 (vs. 19M in 1995)
- $5.4B in spending on allergy drugs in 2009
- 6M workdays missed in 2010 due to allergies
- 16M allergy visits to the physician in 2010
- $17.5B in medical expenditures in 2010 (~$473 per allergy sufferer per year)
I also heard on the radio this morning in St. Louis that now that we passed a no smoking ban we’ve dropped from the worse allergy city to #6.
Peptides, Wnts, and Volume Rendering
It’s always interesting to see information on future developments that are underway (all from Spirit magazine):
- Using a peptide to help you lose weight. Based on research at Indiana University with mice this might be possible.
- Using “Wnts” to heal broken bones faster. Based on work at Stanford University where the stem cells in the bone tissue are stimulated.
- Using volume rendering (ala 3-D movies) to provide images of people innards to help with surgery and diagnosis.
- Using probiotics in smoothies to administer vaccines. Based on research being done at Northwestern University.
Interesting.
The Rider, the Elephant, and the Path
If you haven’t read the books by Chip and Dan Health (Switch and Made to Stick), you should. I was reading a story they had in the Experience Life magazine by Lifetime Fitness the other day. I pulled out a few things here to share:
“For anything to change, someone has to start acting differently.”
Such a simple phrase, but it’s the key of most marketing programs. I was talking to a friend the other day, and he asked why do people bother sending marketing pieces. In today’s world, people know all their options so if they want to change they will. For some people, that might be true (at least on a finite list of things that matter).
In this article, the Health brothers talk about Jonathan Haidt’s book The Happiness Hypothesis where he argues that our emotional side is an elephant and the rational side is its rider. We have to find the balance between the two.
It’s interesting that they talk about the rider as wearing out easily pointing out that exerting self-control and focusing on the next thing to do can leave you worn out. You need to create a path that makes it easier to be successful. This is relevant around adherence. This is relevant for addressing obesity.
All of these articles and books on behavioral economics have fascinating studies in them. In one story they talk about a group of maids which were split into two groups. One group was told that all the work they did cleaning was great exercise. The other group went upon their job as normal. Four weeks later, the group that thought they were exercising had lost an average of 1.8 pounds compared to the other group.
Or they talk about the book Mindless Eating which shows that “people eat more when you give them a bigger container. Period.”
They then introduce 3 surprises which can be helpful in framing messages:
- What looks like resistance is often lack of clarity. Don’t say eat healthier. Say eat more dark leafy greens.
- What looks like laziness is often exhaustion. Change is hard…acknowledge it.
- What looks like a people problem is often a situational problem. Make sure to think about their environment and support system.
Why Aren’t There More Collaborative Practice Agreements?
Collaborative practice agreements (aka collaborative drug therapy management) are legal documents between a specific pharmacist and physician to allow the pharmacist to have more direction in the care of the patient relative to their medications. Given the challenge of the physician to keep up with all the mediations and their lack of access to plan design information and full drug history, I’m surprised that these documents haven’t become more popular.
My guess is that the logistics of a one-to-one legal document around standards of care is complex to scale (see how to set up). But, I always think about how easy this could be for addressing formulary management. The physician could agree to which drugs they considered therapeutically equivalent. They could then tell the pharmacist to choose the drug which was lowest cost for the patient.
Is Royal Pains Good Or Bad For Concierge Medicine?
I really enjoy the show Royal Pains which highlights a physician providing concierge medicine to the super wealthy in the Hamptons. The physician (Hank) and his staff doing an amazing job of diagnosing complex conditions based on a mix of science and deep dives with the patient to really understand their condition, their symptoms, and their environment.
On the one hand, it shows the power of building a relationship between the patient and the physician. It also shows how convenient it can be to have the physician coming to your house and monitoring you.
On the other hand, the type of attention and care shown here with all the technology being available within the home seems unreasonable. The cost to participate would be outrageous (I think).
So, it makes me wonder whether this is beneficial for the whole movement that companies like MDVIP or people such as Dr. Jay Parkinson are providing.
Physicians Want A Long-Term Patient Relationship
In a recent survey by Consumer Reports, 76% of physicians say that a longer-term relationship with their patients would be very helpful.
Is that feasible in today’s environment with consumers more likely to move cities and states?
Assuming it is, this would seem to make EMRs more important especially as they could act as a CRM system for the physician. The average physician probably supports about 2,000 active patients (“physician panel“). It would be difficult for them to remember and personalize their experiences without some mechanism for capturing notes about the patient. Certainly this can and has been done on paper for years, but technology would make this much more efficient.
“A primary-care doctor should be your partner in overall health, not just someone you go to for minor problems or a referral to specialty care,” said Kevin Grumbach, M.D., professor and chair of the department of family and community medicine at the University of California at San Francisco.
The article says that there is research that supports the fact that patients who stick with one physician over time have less healthcare issues and lower healthcare costs. I would assume that it therefore holds that patients who like their physician begin to trust their physician and therefore stay with their physician longer.
Physicians said that respect was the second thing that could help patients get better care. Does that mean that disrespect causes you to get worse care or simply that you’re less likely to engage the physician in a dialogue and understand their recommendation?
There were lots of surprises to me in the data:
- 33% of patients track their changes and activity between visits. I’m guessing those are the chronically ill patients with complex diseases not the average patient.
- 80% of MDs thought that patients would be better off with a family member or friend joining them for the visit…but only 28% of patients have someone with them.
- Only 8% of MDs thought that online research was very helpful with the majority of them thinking it provided little to no value.
- 9% of patients had e-mailed their physician in the past year.
- ¼ of patients indicated some level of discomfort with their physician’s willingness to prescribe medications.
What’s Your Fitness Personality?
If you don’t read Experience Life magazine from Lifetime Fitness, I would recommend getting it or following them on Twitter. They put out some very interesting articles on expercise and food.
One that I found interesting was about Fitness Personalities. By using the Myers-Briggs test as a framework, Suzanne Brue developed 8 different categories (I’m a white). Given the difficulty of making exercise a lifetime habit for many of us, this could be a helpful framework for understanding what works, what doesn’t work, and with some rationale for why.
Here’s the quick summary:
- Blues are safety-conscious, and good at creating their own space and concentrating in a gym.
- Golds are traditional, conservative, and like to share their exercise experiences and results with others.
- Greens are nature lovers who enjoy outdoor activities.
- Reds like to live in the moment and compete in team sports.
- Whites prefer to plan, hate to be rushed and are visionary types who enjoy calm spaces.
- Saffrons like to express themselves as individuals and are attracted to spontaneous, engaging activities.
- Purples are routine-oriented and enjoy repetition.
- Silvers like exercise to be disguised as fun.
Online Company Looking For Pharmacy Partner For Customer Acquisition
A friend I met years ago when I looked at the Duane Reade pharmacy kiosk is now at Everyday Health. He recently asked if I new anyone in the pharmacy area (independent, chain, mail, specialty) that might be interested in partnering with them to drive new customer acquisition based on their online content.
I figure there are several people that might be interested. I asked him to write up a brief note and provide some contact information. Here it is for anyone who’s interested.
Everyday Health is online health network that connects more than 27MM monthly users to in-depth medical content for health condition prevention and management, as well as lifestyle content in pregnancy, diet, fitness, and much more. Our network of 25 sites consists of our flagship, everydayhealth.com, in addition to many well-known health brands such as What to Expect When You’re Expecting, South Beach Diet and Jillian Michaels.
Everyday Health is currently exploring the local health frontier and trying to determine how our organization can better leverage relationships with local doctors, dentists, pharmacies and hospitals. For pharmacies, we’re wondering if there is any value in driving Rx’s to a given storefront and whether there would be economic upside for doing so.
We’d like to connect with people with experience in marketing acquisition of patient Rx’s and/or anyone who can help clarify the above opportunity. Email Dan Wilmer in Everyday Health Business Development at dwilmer at everydayhealth.com.
Intel Health Video On Using Smartphones and Facebook For Health
(Note: Videos and slides may not appear in your e-mail summary. You may have to visit the website to see them.)
Who Should Decide Rx Location – Payer Of Course
Today’s NYTimes article “Pharmacists Fight The Rise Of Mail Order” begs an interesting question. Who should have the right to determine choice?
As the retail pharmacies imply, should they be able to legislate that payers (employers, government, insurance companies, unions) have to allow consumers to come to their location? That seems strange to me.
If the shoe were on the other foot and payers didn’t allow their members to go to mail order, would retail allow the PBM to ask the legislature to change that? (Maybe someone can show me examples of a PBM arguing for mail having to be an option with a client that doesn’t offer mail order.)
Maybe I’m missing something here. Doesn’t the person who is paying the majority of the bill (~80%) have the right to direct care to the lowest cost channel? If someone has an issue with that, shouldn’t it be the consumers talking with their employers?
Shouldn’t competition play out in pricing and value proposition not in the government?
I’ve never heard Chrysler go to the government and say that they had to stop a large employer from limiting their choice of cars for their executive to team to Ford products.
If my employer offers me a discount to Sam’s Club, can CostCo go and argue that with the legislators?
Wouldn’t that turn our whole free-market economy upside-down?
In my opinion, payers should be able to choose their network which could include a limited number of retail locations if that met their expectations on price, outcomes, access standards, and satisfaction. It could include mail or not. BUT, it’s their choice based on the options they have and their management of their spend. Why does government have a role here?
Daniel Pink Video On Drive
I was just visiting Daniel Pink website and saw this video on his book. Good summary plus I love the RSA Animate videos.
RSA Animate — Drive: The surprising truth about what motivates us from Daniel Pink on Vimeo.
You Have Cancer…Blah Blah Blah
After you get diagnosed with a serious disease like cancer or even a chronic condition like diabetes, do you remember anything the physician says? Someone once told me that patients remember something like 12% of what the physician says after that (I couldn’t find the source). Another person shared with me that their physician told them to go home and call them later to talk about all their questions.
This is the extreme example, but a situation that repeats itself day after day. Patients learn that they have a disease. In some cases, they’ve been searching for an answer to their symptoms for a while, and there is a sense of relief followed by anxiety. In other cases, they had a minor problem which leads to identification of a much more serious issue.
I talk about this because in some cases we start this patient on a course of therapy that they don’t understand or a drug which has side-effects they didn’t expect. Health literacy is a big enough issue, but not understanding the receptiveness of the patient based on environmental issues such as shock is a big deal.
We (as a healthcare system) have to continue to help close this gap to educate consumers and leverage the broader care team including physician, pharmacist, and caregivers to help patients understand their condition and the next steps they need to take. Trisha Torrey does a good job of laying out a series of steps for you to take beginning with acknowledging your fear.
Congressional Statements Regarding MTM
In the new Medication Therapy Management Empowerment Act of 2011, there is a nice summary at the beginning of why this is important:
Congress finds the following:
- Medications are important to the management of chronic diseases that require long-term or lifelong therapy. Pharmacists are uniquely qualified as medication experts to work with patients to manage their medications and chronic conditions and play a key role in helping patients take their medications as prescribed.
- Nonadherence with medications is a significant problem. According to a report by the World Health Organization, in developed countries, only 50 percent of patients with chronic diseases adhere to medication therapies. For example, in the United States only 51 percent of patients taking blood pressure medications and only 40 to 70 percent of patients taking antidepressant medications adhere to prescribed therapies.
- Failure to take medications as prescribed costs over $290,000,000,000 annually. The problem of nonadherence is particularly important for patients with chronic diseases that require use of medications. Poor adherence leads to unnecessary disease progression, reduced functional status, lower quality of life, and premature death.
- When patients adhere to or comply with prescribed medication therapy it is possible to reduce higher-cost medical attention, such as emergency department visits and catastrophic care, and avoid the preventable human costs that impact patients and the individuals who care for them.
- Studies have clearly demonstrated that community-based medication therapy management services provided by pharmacists improve health care outcomes and reduce spending.
- The Asheville Project, a diabetes program designed for city employees in Asheville, North Carolina, that is delivered by community pharmacists, resulted over a 5-year period in a decrease in total direct medical costs ranging from $1,622 to $3,356 per patient per year, a 50 percent decrease in the use of sick days, and an increase in productivity accounting for an estimated savings of $18,000 annually.
- Another project involving care provided by pharmacists to patients with high cholesterol increased compliance with medication to 90 percent from a national average of 40 percent.
- In North Carolina, the ChecKmeds NC program, which offers eligible seniors one-on-one medication therapy management consultations with pharmacists, has saved an estimated $34,000,000 in healthcare costs and avoided numerous health problems since implementation in 2007 for the more than 31,000 seniors receiving such consultations.
- Results similar to those found under such projects and programs have been achieved in several other demonstrations using community pharmacists.
Book Review: Drive by Daniel Pink
I just finished the book Drive by Daniel Pink. It’s a great book. I’d recommend it from both a personal and professional perspective because it challenges so much of what we normally think. But, it’s both logical and based on tons of research.
He lays out three reasons why people act:
- Food, water, or sexual gratification (Motivation 1.0)
- Rewards and punishment (Motivation 2.0)
- Intrinsic reward (Motivation 3.0)
The concept of intrinsic reward was new to people. The concept of having this drive challenges all which we believe around incentives. And, his examples reinforce this point. People performed worse on certain tasks when a clear reward was identified.
“When money is used as an external reward for some activity, the subjects lose intrinsic interest for the activity.” Edward Deci
He uses open source collaboration as a great example of this. His example is whether you would have expected Encarta , an encyclopedia by Microsoft, or Wikipedia to succeed. Why wouldn’t a big company with unlimited resources beat out a collection of volunteers?
Business today is based on the whole concept of Motivation 2.0 (i.e., carrots and sticks). He talks about the historical presumption that absent some reward or punishment that people are inert.
“Enjoyment-based intrinsic motivation, namely how creative a person feels when working on the project, is the strongest and most pervasive driver” Lakhani and Wolf
He goes on to explain the difference between algorithmic and heuristic problems. Algorithmic problems can be solved based on a single path while heuristic problems have different options. [It’s like when I went to business school and architecture school.] He quotes a McKinsey study which says that 70% of job growth in the US is around heuristic work. Therefore, applying a traditional model of motivation to creative work creates a major issue. It turns creative work which we feel passionate about into a disutility (something we won’t do without payment).
Now of course, creative “work” isn’t “play” if the basics aren’t addressed – i.e., fair pay. This has application in lots of areas including how we get kids to learn. Paying kids for specific activities pushes them to focus on completing those but not necessarily learning how to apply the knowledge. I think it’s a key issue which should be getting debated in when, if, or how to use incentives in health care. This is why you may see a short-term improvement that falls off over time.
This will be very relevant as P4P becomes more important. If rewards narrow the focus of solutions and limit creativity, will that be good in that it focuses people on specific processes? Or will it be a problem because in complex cases or cases where there are alternatives, the creativity of solutions and consideration of options will be limited?
But, he’s careful to make sure you don’t think that rewards are always bad. They have to be used appropriately and for the right tasks.
“If we watch how people’s brains respond, promising them monetary rewards and giving them cocaine, nicotine, or amphetamines look disturbingly similar.” Brian Knutson
He lays out “The Seven Deadly Flaws” of using carrots and sticks:
- They can extinguish intrinsic motivation.
- They can diminish performance.
- They can crush creativity.
- They can crowd out good behavior.
- They can encourage cheating, shortcuts, and unethical behavior.
- They can become addictive.
- They can foster short-term thinking.
He suggests that for tasks that don’t inspire passion nor requires deep thinking that there are three things that are important:
- Offer a rationale for why the task is necessary.
- Acknowledge that the task is boring.
- Allow people to complete the task their own way.
He talks about how using bonuses can work even for creative tasks when it’s not an “if-then” reward, but it’s a “surprise”. (Which is hard to repeat multiple times.)
He goes on to talk about Type A personalities. Theory X and Theory Y. Type I and Type X. It makes some key points about how we perceive people. Do we believe in the “mediocrity of the masses” or do we believe in people’s interest in succeeding? This is where Motivation 3.0 begins to come in and there is a focus on people’s desire to success or to master something.
He makes a lot of points that remind me of Malcolm Gladwell’s book Outliers. Mastery is hard work.
“The most successful people, the evidence shows, often aren’t directly pursuing conventional notions of success. They’re working hard and persisting through difficulties because of their internal desire to control their lives, learn about their world, and accomplish something that endures.” (pg. 79)
He talks about how these frameworks can be applied at an organizational level and cites a Cornell University study of 320 small businesses. Those that offered autonomy grew at four times the rate of control-oriented firms and had one-third the turnover. He talks about ROWE (Results Oriented Work Environment) and gives examples of companies that really give their employees freedom. It’s a radical change for many people…imagine a work environment where you set your own hours.
He introduces the concept of “flow” from work by Csikszentmihalyi which was new to me. It describes this state where people are challenged but have an opportunity to stretch to get there.
He talks about mastery as a mindset and how what people believe shapes what people achieve. This belief is critical especially in addressing things like obesity (my opinion) and plays into a lot of what you see on The Biggest Loser. Losing weight (mastering being in shape) is a lot of work, and you have to believe you can do it. You also have have to have some motivation other than financial goals.
There is an interesting discussion of “entity theory” versus “incremental theory” which talks about whether you believe you have a finite intelligence or an opportunity to expand your intelligence. There is lots of talk about education in the book which I think is really important. Are we creating kids that want to “prove their smart” by getting A’s or who are really trying to learn?
“West Point grit researchers found that grittiness – rather than IQ or standardized test scores – is the most accurate predictor of college grades.”
He has a whole chapter on purpose. I think this is key to healthcare. He talks about autonomy and mastery, but without purpose, we don’t have balance. Think about someone who is obese. They want to be autonomous and master being in shape, but when you listen to them talk, it is typically a focus on being there for their family that motivates them to actually take action.
He made me wonder about linking health outcomes to lower costs (i.e., value based). If I know that my healthcare premiums go down if I manage my BMI or cholesterol or get certain tests done, am I just checking a box or am I really changing my lifestyle in a sustainable way?
Social Media Analysis – The Involved Patient
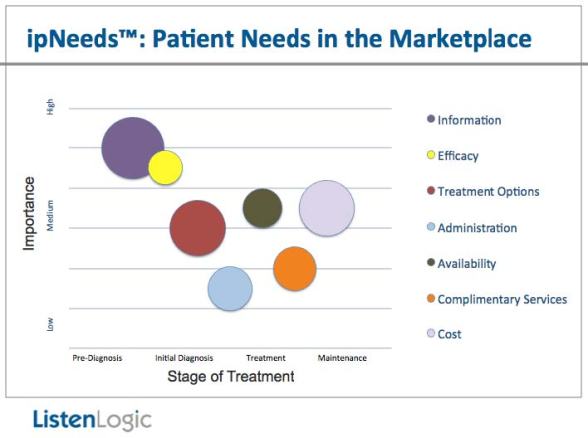
I just finished reading a whitepaper by ListenLogic Health. They do social media analysis for pharmaceutical companies on what patients think. There is some interesting data in there looking at what people talk about based on age. They also show several charts about information searched for or discussed by stage. I pulled out one chart from their whitepaper to share:
They also share some data on what patients say they want from physicians. This is things like explaining their data better, helping them understand their options, and all basically focus on engaging them.
Can We Use Technology To Address Gaps In Resources – YES!
Dr. Joseph Kvedar writes a great piece about the psychology of persuasion and the possibility of using technology to engage consumers and drive behavior change. This is an important topic as we look at addressing healthcare as a country. Since behavior and consumer choice drive a significant portion of our healthcare costs, we have to think more about how to engage patients – what is the right message? what is the right channel? what is the right time to deliver the message?
We can deploy technology in smarter to ways to engage consumers in new ways that leverage our limited resources in better ways – i.e., get good and scalable outcomes without increasing costs. That is what we do everyday at Silverlink Communications with our clients whether it’s around HEDIS, adherence, condition management, or many other programs. Recently, there was an article in Time Magazine that talked about some work we did with a Medicare population for Aetna.
I also think you can look at the research Stanford has published on the topic over the past decade. You can also look at some of the data from the CVS Caremark Pharmacy Advisor program. While it certainly showed the value of having pharmacists involved, it also showed some positive results from automation.
The reality is that combining automation and live resources can be very powerful. Technology can screen and triage people to connect the at risk population with critical resources. This can allow resources to support as many as 4x as many consumers.
Words Matter: Have You Drugged Your Kid Today
I think I’m going to start a series tagged to “words matter” where I call out some of the examples that I notice. The first one is the story about a teacher getting fired for her bumper sticker on her car. (Something I never thought would happen.) Her bumper sticker said “Have You Drugged Your Kid Today”.
First off, I think people are entitled to their opinions.
Second, I think we all would agree that there are certainly times when patients are given medications rather than ask to change.
Whether kids are over-medicated today versus the past is hard to know. We are certainly more aware of conditions these days, but I think this is a hot topic. Just look at some of the articles on the topic.
- New Yorker Magazine on kids and medication
- Article on the growing number of kids on medications
- Huffington Post on whether kids should be on these medications
- Article on whether we take too many mind altering drugs
It’s not like the teacher was taking some massively controversial position. She wasn’t teaching the kids. She was simply expressing an opinion on a hotly debated topic in a quick sound bite which she put on her car in the form of a bumper sticker.
The Benefit’s Package Blog Carnival
I appreciate the submissions that I got for this week’s Benefit’s Package Blog Carnival.
Adam Fein of Drug Channels submitted a post that was near to my heart since it is a study that everyone has been talking about (in the pharmacy space). He wrote up a summary of the research that CVS Caremark published about choice of retail versus mail and what they were seeing. Like adherence, past behavior is a good indicator of future behavior. In this case, people who had used mail before, were more likely to use it again.
In Dave Kerrigan’s submission, he talks about the need to Percolate the Perks. He brings up a great point around how to sustain engagement. The reality of differentiating your benefits, keeping people aware of them, and getting people to use them is a real challenge. Some of the ideas he brings up are relevant across the spectrum of engaging consumers.
Building on engagement, one of the things that scares a lot of people is being misdiagnosed or given the wrong treatment (or getting surgery on the wrong body part). Evan Falchuk talks about this in his blog post on Third Place Health Care. The opportunity to get a 3rd party opinion is one that I think lots of people would like to access. And, interestingly, Jennifer Benz also talks about this in her submission about Boosting 401k Participation. Her post talks about what’s happened from a tax perspective and stressing that with the consumer.
While I’m not sure of the relevance from a health benefits perspective, I did get an interesting submission from the Action For Better Healthcare blog on what Geisinger is doing around making facilities more efficient. This plays into a lot of the green architecture efforts that are ongoing (see a blog and book from a classmate of mine from architecture school). But, I found another post on the blog more interesting –an interview they posted with Karl Rowe which is interesting given the Kaiser research that many people think healthcare reform is already repealed.
Next up, I thought the Free Range Communication blog does a great job of breaking out highlights from the recent SHRM report. A lot of topics of focus to the HR community are very health centric, and a lot of the trends around aging, increased use of caregivers, more people with chronic conditions, etc. are all very relevant. For those of you looking for similar data around pharmacy benefits, I just pulled out some data from another report from PBMI here.
Dr. Liu wrote on Why Consumer Driven Healthcare Will Fail and also had a piece on the recent Consumer Reports story about What Doctors Wish Their Patients Knew. He draws some parallels around CDHC and 401k plans which I think is very relevant.
Another post from this past week that I liked was Dr. Val’s write-up on Tabloid Medicine. Given the fiasco around vaccines and the false research, this should be a hot topic.
I also liked an AMA story about Secret Shoppers and Susannah Fox’s video and writing on Healthcare Out Loud. A few other things from this week were a brief summary of some of the work Sanofi-Aventis is doing in social media, a paper on The Connected Patient by Jane Sarasohn-Kahn, and some research on storytelling and hypertension.
The Cost Of Chronic Pain
The March 7th edition of Time Magazine has a whole section on chronic pain including a fascinating timeline of how pain has been managed over the years. It’s just in recent history that pain has moved from being a side effect to being a condition to be management.
An article by Dr. Oz provides some statistics on pain:
- The annual price tag of chronic pain is $50B.
- Lower-back pain is one of the most common complaints affecting 70-85% of adults at some point.
- 7M people are either partially or severely disabled because of their back pain.
- Lower-back pain accounts for 93M lost workdays every year and consumes over $5B in costs.
- 40M Americans suffer from arthritis pain.
- 45M Americans suffer from chronic headaches.
- People with chronic pain are twice as likely to suffer from depression and anxiety.
One of his key suggestions – if you’ve worked with your physician for six months and its not resolved – go see a specialist.
He also points you to the American Chronic Pain Association for communication tools in helping you verbalize your pain.
In his article and in the other articles, it talks about stretching as a way to alleviate pain. Obviously, there are medications that can help with pain relief although some of them can be abused and addictive. And, both Dr. Oz and the other articles mention acupuncture as a potential solution.
You can also go to the American Chronic Pain Association to learn more.
From a management space, one of the areas where chronic pain is a big area of focus is in Worker’s Compensation. For more about this space, you can follow Joe Paduda’s blog. You can also follow some of the Worker’s Compensation PBMs such as:
Pharmacy Benefit Data From PBMI
I had a chance to read through the new 2010-2011 Prescription Drug Benefit Cost and Plan Design Report that PBMI puts out and is sponsored by Takeda Pharmaceuticals. Here are some of my highlights:
-
Percentage of the pharmacy claims costs paid by the beneficiary
- Retail = 25.3%
- Mail = 20.1%
- Specialty = 15.9%
-
Average difference between retail and mail copayments (see chart):
- Non-preferred brands = $18.38
- Preferred brands = $7.15
- Generics = $3.61
-
5.1% of employers are covering genetic tests to improve drug therapy management
- 68.8% of them are covered under the medical benefit
- 43.0% of employers are restricting maintenance medication dispensing to select pharmacies (retail or mail) [much higher than I expected]
-
They give examples of the percentage of respondents using the following value-based tools:
- 31.7% – reduced copayments in select classes
- 19.7% – incentives to motivate behavior change
-
I was surprised to see a significant drop in the percentage of clients requiring specialty medications to be dispensed at their PBM’s specialty pharmacy.
- 2009 = 53.8%
- 2010 = 40.0%
- There was a similar drop from 15.7% to 11.5% of employers restricting coverage of specialty drugs under the medical plan.
- Given all the focus on medication adherence, I was disappointed to see that only 24.2% of employers were focused on maximizing compliance in specialty. [Maybe they haven’t seen all the studies on this topic.]
- They have some nice comments on Personalized Medicine and the critical questions to address.
- I was also surprised that less than 1% of employers were using onsite pharmacies or pharmacists.
-
They provided the following data on average copayments for 3-tier plan designs with dollar copayments:
- Generics at retail = $9.45
- Generics at mail = $19.06
- Preferred at retail = $25.93
- Preferred at mail = $53.63
- Non-preferred at retail = $46.43
- Non-preferred at mail = $98.25
-
The average pharmacy discounts (based off AWP) were:
- Retail brand = 17.5%
- Retail generic = 46.6%
- Retail 90-day = 19.8%
- Mail brand = 23.3%
- Mail generic = 53.5%
- Specialty = 18.7%
- The one number that seemed off to me was the Rxs PMPM which they had as 2.29 for active employees. That would mean 27.48 PMPY which seems closer to Medicare. [I typically use 12 Rxs PMPY for commercial and 30 Rxs PMPY for Medicare as a quick proxy.]
-
For the first time, they showed the percentage of employers excluding coverage of non-sedating antihistamines (e.g., OTC Claritin) and proton pump inhibitors (e.g., Prilosec OTC). Both classes have had lots of blockbuster drugs go OTC (over the counter) so it makes sense to exclude coverage.
- NSAs = 44.7%
- PPIs = 30.6%
- They provide a nice summary of how employers are using UM (utilization management) tools.
The report has tons of data on different scenarios, different plan designs, rebates, and many other topics. I’d encourage you to go online and read thru it.
BTW – The respondent group of employers included 372 employers representing 5.8M lives including both active and retired. The average group size (active only) was 9,736 which is a decent size employer group. And, 12% of the respondents were part of a union bargaining agreement.

 March 20, 2011
March 20, 2011