Much like the soda PSAs being used in NY, a friend at work suggested this as a pointed message around diabetes. A little extreme perhaps, but I thought it was good.
10% Discount On DMAA Registration
As a speaker at the upcoming conference, they sent me a discount code…
Register Now for The Forum 10
DMAA: The Care Continuum Alliance, the leading trade association for wellness, prevention, disease management and other services across the continuum of care for chronic conditions, invites you to its 2010 annual meeting, The Forum 10, Oct. 13-15, in Washington, D.C. Join leading health plans, wellness and care management organizations, physician groups, health IT companies, state and federal programs and other stakeholders as they discuss health care reform, share best practices and network. Keynote speakers include best-selling author and motivation and engagement expert Dan Pink; and a panel presentation by nationally recognized consultants on workplace wellness strategies. View complete programming details
Special Registration Offer: Viewers of this notice can receive 10 percent off standard Forum pricing by using discount code “FRIENDS-FORUM” during the registration process. Go to online registration
Choices: Grande Skim Mocha With Whip @ 140 Degrees
Choices. We can all become overwhelmed with them. As several studies have shown, more choices are not better…they paralyze us and limit our ability to make a decision.
So what do we do with this. Choice is a double-edged sword. On the one hand, you want to offer choice to everyone. On the other hand, this can make implementation very difficult.
Like my Starbucks example. I can customize almost everything off a pretty basic menu…even the temperature. (BTW – they suggested using 140 degrees rather than saying kiddy temperature) But that makes it more difficult to standardize and should increase the risk of error. Imagine doing this efficiently and in scale.
Mass customization has been a challenge for years.
People can have the Model T in any color – as long as it’s black. (Henry Ford)
While technology allows this to a certain degree, it all has to be moderated. Let’s take communications. I could let every consumer tell me their preferences and other facts about them.
I want you to send me automated calls unless the information is clinical in which case I want a letter than I can share with my physician. I’d like the calls made to my home number between 5-7 pm or on Saturday’s between 10-4. I’d like you to leave a message and don’t call back unless I don’t act for seven days. If I interact with the call, please text me the URL or phone number for follow-up. I like to be addressed by my first name. I’m an INTJ so please use that as for framing the message.
You get the point. Where do you stop? And, do you really think that I know what’s best. I tell almost everyone to e-mail me, but depending on when it comes in, it could be days before I respond or even read the e-mail. That’s if it passes the spam filter.
I’m sure if I asked 10 people whether they wanted automated calls then 7 of them would say no, BUT you know what…good calls work (voice recorded, speech recognition, personalized). The vast majority of people interact with good, automated calls (some for 10+ minutes). Most people think about those annoying robocalls that use TTS (text to speech) we all get around the elections. But, good technology with a relevant message from a relevant party get people to care. It’s all about WIIFM (what’s in it for me). The other half of the equation is being able to coordinate the multiple modes. (e.g., I missed you so I’m sending you a letter. Let me text you the URL.)
So, should I let the consumer pick their preferences? Sure for certain things. But, what about a drug recall (for example)? Do I have to wait a week to get a letter? What can I personalize versus what should the company own. I pay for them to “manage” my health. Why don’t I let them?
There is no perfect system. You need a series of things to be successful.
- A database to track consumers – demographic data, claims data, preferences, interaction history, …
- A workflow engine with embedded business rules to manage communication programs with rules about what to do when certain situations arise
- Reporting to track basic metrics
- Analytics to understand and analyze programs
And, of course all this requires expertise to interpret and leverage the data for continuous improvement.
Are you doing all that? I doubt it…but you can be.
Doctor – Patient: Relationship or Transaction…and Therefore

Don’t jump the gun too quick here. I assume most of you are going to say that there is an implicit (or explicit) relationship between the physician and the patient. They have some interest in your outcome and your care.
But, before you go there, I want to put forth a hypothesis. If this is true, is it okay for the physician to monitor your activities on your social network? (original question posted by The Side Note blog) Can they follow your tweets? Can they review your activities on Facebook or MySpace or some future site? Can they reach out to you to ask why you tell them you’re on a diet while you tweet about eating a Big Mac? Can they ask you about side effects that you’re having to a medication?
I’m positive that they don’t have the time to monitor these sites (but someone could do that for them). The question is whether it’s ethically okay for them to do that and use that information to provide you with care.
It seems like everyone else is using that information (which is public domain). Lawyers are using it. Tax collectors are using it. HR managers are using it. I would assume insurance adjusters might be using it.

How To Improve Your Presentations
I’ve been asked many times how to improve your presentation skills. I don’t have any hints about visualizing the audience naked. My perspective has been practice, practice, practice. I think it fits well with the Outliers concept of 10,000 hours.
When I was in high school, I participated in Model United Nations (MUN) which was a great experience and forced you to get up in front of your peers and present on a topic. You had to research a country and understand their perspective. That was good, low pressure experience.
In undergraduate school, I studied architecture and you had to constantly stand in front of your peers and judges to present your solution. In business school, I constantly presented our cases and other work (until my teachers said I couldn’t present any more). Then, I think what finally helped me hone my skills was Toastmasters. A friend got me into it in graduate school, and it was great. We dropped pennies in glasses if people used “uhms” in their presentations. We did ad-hoc presentations on topics that we didn’t prepare for. We had to present in different ways using different skills.
Then, at Ernst & Young LLP, we practiced everything and focused on details. What does a white shirt under a dark suit mean versus a grey shirt under a grey suit? Attention to details.
At Express Scripts, Larry Zarin (CMO) introduced me to Presentation Zen before the book was even out. Before our annual Outcomes conference, we would practice our delivery over and over again. We would focus on slide content, fonts, and everything else that made them easy to use.
There are lots of things to think about in driving presentations, but in the end, I think there are some basics that I live by which are only learned and honed by practice. (I also think that presenting is highly correlated with being able to facilitate meetings (see good list here).)
- Tell them what you’re going to tell them. Tell them what you want to tell them. Tell them what you told them.
- Have a structure to the presentation. Think Minto Pyramid Principle or writing a good letter (intro, body, conclusion).
- Know your audience. What’s important to them? What’s their history with the topic?
- Manage your environment. How do people sit? Projector or handouts?
- Engage people…don’t just lecture to them.
- If you’re using slides or handouts, make sure people can read them and understand them.
- Slides are NOT handouts. They are props.
- Don’t talk to the slides. Make eye contact.
- Walk thru the presentation (at least once) out loud before delivering it to your audience.
- Have a routine (like golfing). I like to get a good night’s sleep and run in the morning before any big presentation. I also try to manage my caffeine intact before the presentation.
I could go on, but those are some thoughts.
Health Loyalty Lessons
Colloquy published a good article on Health Loyalty Lessons. It pointed out 6 things that were important:
- Short-term incentives can mean long-term payoffs.
- Understand your objectives if you want to offer the right benefits.
- Communicate. Communicate. Then communicate some more.
- Strike a balance between hard and soft benefits.
- Stay relevant if you want consumers to stay motivated.
- Raise the bar.
These are good points (and more detail is in the article). They’re relevant whether you’re doing a full blown loyalty or incentive program or simply focusing on the WIIFM principle (What’s In It For Me). This is why healthcare communications is such a hot area right now.
- Who do I communicate with? (targeting)
- When do I communicate with them?
- How do I communicate with them? (letter, call, e-mail, text)
- What message will drive them to act?
- How do I measure success?
- What’s worked before…for the individual or for people in the same segment as the individual (gender, age, condition, income, plan design)?
No “Pay-to-Delay” For Pharma
The Senate Appropriations Committee approved adding language to restrict this practice to a spending bill. Will it ultimately pass? I’m not sure.
What is it? The way a generic drug comes to market is that generic manufacturers (e.g., Teva) will wait for a patent to expire and/or challenge the patent. They do this by filing an ANDA (Abbreviated New Drug Application). Manufacturers obviously want to enjoy the exclusivity of their patent(s) as long as possible.
My understanding is that “pay-to-delay” is when:
- The brand manufacturer knows that someone is going to challenge their patent and try to get a generic to market before the patent expires. They pay the generic manufacturer not to do this and in return might allow them to offer an “authorized generic” before the patent expires.
On the one hand, my reaction to this potential legislationis a “finally”. On the other hand, this is a defeat for creative capitalism. Does a company have to launch a product?
If Ford wanted to pay Toyota to delay the launch of a new car such that they both made more money, would the government step in and tell them they had to launch it. Perhaps that’s apples to oranges.
The problem here is that while the brand manufacturer made more money and the generic manufacturer made money for doing nothing (other than getting the right to launch it) the public (i.e., consumers) and payers lost since they had to wait to save money.
Is This The Time To Buy Pharma and Biotech Stocks?
Certainly there’s been lots of press about their P/E ratios being historically low especially at some of the blue chips like Pfizer. There are good reasons like limited pipelines and generic competition. And, generally, my opinion is that if everyone’s talking about it then you’ve missed your window.
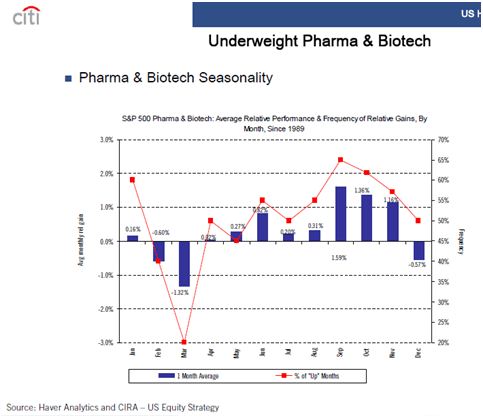
That being said, I found this chart very interesting. It came out from Citigroup months ago, but if I interpret it right than it shows a typical uptick in those stocks in the upcoming months. [Note: This should not serve as investment advice but simply presentation of data. Any investments should be made based on your own research and the advice of your advisors.]
If it’s hard to read, the title says “S&P 500 Pharma & Biotech: Average Relative Performance & Frequency of Relative Gains, By Month, Since 1989”. So, in September, these stocks have gained an average of 1.59% with a frequency of 65%.
A Collection Of Misc Articles
I’m in a clean-up mode in my e-mail and blog pile. For the first time in almost two years, I’m beginning to feel caught up. I have less than 250 e-mails (combined) in both my personal and work e-mail inboxes. This is a lot since once I open an e-mail I either (a) delete it; (b) respond immediately if possible; (c) file it in a folder on that topic; or (d) leave it in my inbox for future reading (i.e., it’s too much info to digest quickly) or for future response (i.e., it requires more time than I have).
It always begs the question of how late can you respond to something. Yesterday, I stumbled upon a e-mail from someone in Europe that wanted me to add their pharmaceutical site to my blogroll. I clicked on the link, reviewed the site, and added it. It took me less than 5 minutes, but the kicker was that he e-mailed me almost a year ago.
*****
- A study by Timothy Monk at the University of Pittsburgh concluded that keeping children on a stable schedule of activities can make them less anxious as they grow up.
- People with strong social connections are 50% more likely to live longer.
- People who regularly logged in to a weight-management website for 2 years lost 9-pounds (3x those that didn’t log in).
- Can a mouthguard make you a better athlete?
- A study in the July Health Affairs says that patients that use e-mail with their physicians have healthier outcomes. (Lots of challenges here, but this should be key in health reform.)
- Digital Darwinism…you have to develop relevance, interactivity, and accountability.
- MyPressurePoints.com – a survey and website focused on African-Americans with diabetes.
- Generic drug videos from Teva.
- 9 Leading Trends in Rx Plan Management by Medco.
- Two low-cost generics used by Kaiser to reduce heart attacks and strokes.
- Managing with the Brain in Mind – neuroscience.
- AMA and Medco study about physicians and pharmacogenomic testing
More to come…
Back To The Future: The Role Of The Pharmacist
Between the focus on differentiation and the focus on adherence, we have seen (and will continue to see) greater use of them as a strategic asset. CVS Caremark is leveraging them in their Pharmacy Advisor solution. Walgreens continues to leverage them at the POS. Medco is using them in their Therapeutic Resource Centers. And, the independent pharmacists have stressed this story for years.
In Medicare, the Medication Therapy Management (MTM) process begins to recognize the power of pharmacists and actually rewards them for their efforts. I was quoted in Drug Benefit News today about this topic. Here were a few quotes:
“The pharmacist is an under-utilized resource today,” George Van Antwerp, vice president of the Solutions Strategy Group at Silverlink Communications, tells DBN. “They go to school to work with patients and often end up simply filling bottles.”
While the benefits of pharmacist intervention are undeniable, Van Antwerp says, the challenge is finding the right balance of face-to-face interaction and automation. Issues also include getting a good return on investment for such services by condition and the fact that only an estimated 60% of the people picking up prescriptions are the patients themselves. In addition, “the staffing model right now would be stressed if pharmacists were spending significant time on cognitive services,” he maintains.
Aetna To Outsource PBM Functions To CVS Caremark
While the market seems more mixed on this than me, I see this as a good thing for CVS Caremark. If played right, this could be a huge factor for 90-day retail and/or Maintenance Choice since Aetna (as the payer) will have huge incentives to take advantage of this.
I was a little surprised since most of the rumor had been that Medco was going down this path with Aetna and that this was what they had pitched to Wellpoint prior to the Express Scripts acquisition of the pharmacy business.
And, for those of you that have been around this space for a while, you might remember that Aetna did outsource some of their PBM business up until about 6 years ago when they insourced in from Express Scripts. I’d be interested to understand what changed (which might simply be in the finer points of this new agreement which doesn’t appear to sell assets but to leverage CVS Caremark’s scale).
It clearly points out that there are scale efficiencies in the PBM business something that I think will come to end in the near future (as predicted in my white paper a few years ago). So, I think the question a lot of people are asking is whether this move will accelerate different models to get to scale:
- A roll-up strategy of smaller PBMs by the large PBMs.
- A consolidation of smaller PBMs into coalitions and buying groups.
- Smaller PBMs contracting with larger PBMs for core services.
Let’s look at some of the PBM functions to think thru what makes sense to consolidate and leverage (IMHO):
- Sales – independent
- Marketing – independent although some physician or consumer marketing could be consolidated
- Implementation (Client Set-Up) – independent
- Research – drug trend, research studies, and analytics could be consolidated
- Plan Design – could be consolidated but not likely large efficiencies
- Drug Acquisition – consolidation would drive the majority of value
- Procurement – consolidation could add value
- Rebating – another big opportunity for consolidation but requires coordination on formulary (P&T) and other areas
- Mail Fulfillment – should offer consolidation benefits
- Call Center – should offer consolidation benefits
- Claims Processing – limited but possible consolidation benefits
- Clinical Reviews – easy to consolidate but minimal savings
I think given Express Scripts and NextRx and now CVS Caremark and Aetna (although different relationships) that this puts the spotlight back to Medco for the next move. I think the likely focus areas would be on Cigna and Prescription Solutions (part of United Health Group). After those two, there are other less likely targets – Prime Therapeutics, Walgreens (PBM), and MedImpact.
Drive: The Surprising Truth of What Motivates Us
I haven’t read the book yet, but this is a great video. I love the fast paced whiteboarding to match the speaking.
DMAA Client Presentations
We (Silverlink Communications) are very excited to see three of our clients get selected to present at DMAA this year. That is a tribute to all their hard work, creativity, inspiration, and willingness to leverage technology to improve outcomes.
Here are the presentation summaries from online:
Reducing Blood Pressure in Seniors with Hypertension Using Personalized Communications
CONTINUUM OF CARE SERIES
Wednesday, Oct. 13, 1-2 p.m.
- Examine how an integrated communications program that utilizes remote monitoring and interactive voice response components combine for an easily scalable, cost-effective solution to reduce hypertension.
- Review a program where 18 percent of participants transitioned their hypertension from out-of-control to well or adequate control.
- Identify best practices for how personalized, automated, interactive communications can be leveraged to control hypertension in a scalable manner.
- Evaluate how high blood pressure readings alerted patients with immediate feedback and education to help them better manage hypertension.
Improving Statin Adherence through Interactive Voice Technology and Barrier-Breaking Communications
Wednesday, Oct. 13, 2:15-3:15 p.m.
- Examine how interactive voice response (IVR) and barrier-breaking communications can measurably improve statin adherence.
- Review key barriers to statin adherence, including several barriers that are more significant than cost.
- Identify best practices for using IVR technology to improve statin adherence by addressing specific barriers.
- Evaluate how continuous quality improvement processes were used to drive higher response rates to IVR prescription refill reminder calls.
Addressing Colorectal Screening Disparities in Ethnic Populations
Thursday, Oct. 14, 12:30-1:30 p.m.
- Examine how interactive voice response (IVR) technology and personalized messaging improves the rate of colorectal cancer screening for different populations.
- Review the impact of ethnic-specific messaging on colorectal cancer screening rates and how this differs by ethnicity.
- Examine how engagement is influenced by the gender of the voice in communications outreach.
- Identify how to use predictive algorithms to project race and ethnicity to support tailored communications.
National Drive-Thru Day…and Pharmacy Impact
I know…I know. I’m reminding you late. It was July 24th. I’m sure it would have changed your plans for the day. (Who makes up these days?)
I do think the drive-thru is interesting for several reasons:
- What it says about us overall; and
- It’s impact on the pharmacy business.
In general, there aren’t many healthy uses of the drive-thru. It’s a productivity tool that (like technology) limits our interactions with other people.
A few facts for you:
- We spend $110B at drive-thru fast food restaurants each year.
- The first drive-thru fast food restaurant was at In-N-Out Burger in 1948.
- Strangest use of a drive-thru (IMHO) was Gaitling’s Funeral Home in 1989.
- In the mid-2000’s, drive-thru staffing was changed such that the order taker could be outsourced to allow the person taking your money to be more productive (i.e., you’re talking to a person at a different location).
So, what’s happened in pharmacy? I’ll have to find the date of the first drive-thru in pharmacy.
- Walgreens certainly seems to be the dominant user of this strategy where they will typically have 1-2 lanes for drop off and pick-up of prescriptions. This is definitely a productivity play for the drive (suburban) culture. I’ve used it frequently when I have a first-fill and either kids in the car or it’s raining or cold.
- 29% of people said they use this method in a WilsonRx 2008 study…but only 3% said they prefer this method.
- 42% of people who used the drive-thru were highly satisfied (compared to 56% highly satisfied with either pick-up at the store or receiving by mail).
The big question a few years ago was whether this productivity enhancement damaged the pharmacist-patient relationship. I would argue “of course it did”. How could it not? You no longer talk to them face-to-face.
I would also question privacy here. On the one-hand, it’s harder for the patient’s behind you in line (i.e., in their car behind you) to eavesdrop. BUT, when there are two lines, it seems pretty easy for the car next to you to hear everything you talk about with the pharmacist. AND, if we’ve learned on thing from mobile phone headsets, it’s that people seem to talk louder into the phone (i.e., I think the pharmacist inside is talking to you louder).
Of course, one true question is whether you really had a relationship with the pharmacist to begin with. In most cases, you’re dealing with a pharmacy tech not the pharmacist. The majority of people (even at independent pharmacies) don’t know the first name of their pharmacists (BTW – mine are Marc and Renee).
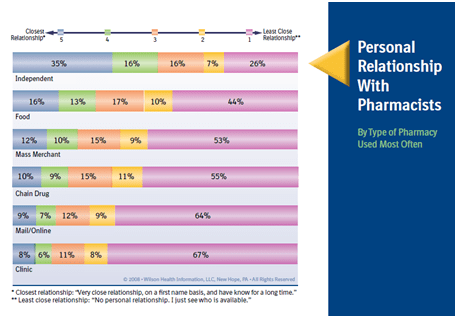
Now, what I find most shocking in this chart from the 2008 Pharmacy Satisfaction Digest by WilsonRx is that only 1% more know the name of their pharmacist at a chain drugstore than at mail order.
Being Proactive and Reactive Improves Adherence
I don’t think any of us who spend a lot of time in the adherence area are surprised by this, but it’s always good to have a nice, published study to reinforce the point.
CVS Caremark published a study done last year using interactive outbound call technology to improve their adherence program. (Chang et al., Improving Persistency for Maintenance Medication Therapy Through an Interactive Voice Response Program, Journal of Managed Care Pharmacy, 2010. 16 (2): page 156.) It showed that being proactive (i.e., calling before the patient ran out of pills) was better than doing nothing (control group) and better than calling reactively (i.e., the patient has run out of pills). But, if you do both, you significantly improve the likelihood of them getting a refill and staying adherent.
Caremark iPhone App – Will Others Follow?
CVS Caremark announced today that they were releasing a Caremark iPhone application. First, I think it’s about time (for some PBM to do this). I would think the other PBMs will follow suit.
Second, I think this is a great opportunity for an expanded CVS Caremark iPhone application which expands the functionality of the app and is like Maintenance Choice in that it offers a benefit of the integrated company.
Today’s application is PBM centric and focused on ordering refills (I assume at mail only); checking prescription order history (I assume mail only); viewing prescription history; requesting a new prescription (retail-to-mail I believe); checking drug cost; and finding a nearby network pharmacy. Checking drug cost could be the coolest feature since it would give patients what they don’t have today – an ability to check the cost while they’re at the physician’s office. Finding a network pharmacy is an important tool if companies were to promote limited networks, but it’s only a nice to have if all the pharmacies are in the network.
So, of course the question that I would have is when will they add the retail components to request retail refills (at CVS stores or all locations); check status of prescriptions (e.g., prior auth required); request a renewal of an Rx; request a lower cost alternative; find a CVS with a MinuteClinic; or identify opportunities to save money (e.g., a generic alternative).
There are lots of other things to push out via the application, but I agree with the strategy of focusing on the core applications first. Caremark (or other PBMs) could push clinical suggestions; send adherence reminders; do satisfaction surveys; collect barrier data (why not adherent); and collect information (why not using generics). I also see it as a great way to push tools – e.g., 5 questions to ask your physician when you get a new Rx.
It would be interesting to see the statistics in a year – how many downloads of the app; how frequently is it used; patient satisfaction with the Caremark for those with the app (vs those without); adherence for those that use the application; what functions work best; savings versus other modes of communication; and effectiveness of their appliction versus other health applications.
How Much Do You Really Notice?
The Dateline NBC show “Did You See That” shows us just how little we see or how easily our minds are distracted. This is a real issue when we think about communicating information to patients who have hundreds of other things going on in their life.
Would you notice if the man who stopped to ask you directions on the street all of a sudden became a woman?
Would you notice a man walking thru a group of basketball players when you were focused on counting passes?
Would you notice when the talk show host’s shirt turned from blue to green?
Would you notice that the person helping you at the store was blond one minute and a brunette the next minute?
People in the videos on the show didn’t. It was amazing…scary…surprising.
It makes you think. It made me want to experience the tests. Would I notice?
Watch this video – http://www.msnbc.msn.com/id/21134540/vp/38287250#38287250.
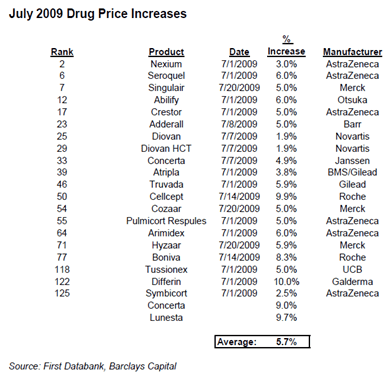
Brand Drug Prices Continue To Go Up
As Medco highlighted several weeks ago, brand prices are going up a lot faster than generic prices. That’s nothing new. But, Barclays Capital recently highlighted that brand prices are going up faster in 2010 than any prior year (based on First Databank data).
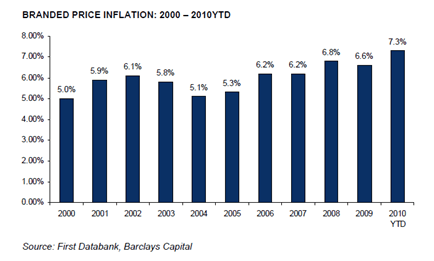
Why?
- Are they trying to make up for their concessions around Part D pricing and closing the donut hole?
- Are raw material prices up?
- Is it harder to develop a blockbuster drug and therefore R&D costs are going up?
- Is it because the brand market is so much smaller with generic fill rates up?
- Is it because their drug is losing patent?
- Is it because they’re chasing more orphan drugs?
I’m not sure, but it certainly is a point of concern for many plans although in the big picture it’s not a huge driver of cost…
- Prescriptions represent 10-15% of total healthcare costs.
- Brand drugs represent 20-30% of prescription claims (but probably 70-80% of prescription costs).
- Even a 10% increase in prices across the board would only be about 1% increase in total healthcare costs.
10 Numbers You Need To Know For Mobile Health
I found this great list of statistics yesterday from RxEOB. I won’t repost them all here so you click thru to the original content, but I thought it was very helpful.
23%. Percent of American households who use only a mobile telephone, no land line. Another 15% of homes with landlines report they receive all calls to their mobile device.
32%. Percent of Americans whom have accessed the internet from their mobile phone as of 2009. (19% reported they did it “yesterday”). In total 56% of Americans have accessed the internet via some form or wireless device (e.g., phones, MP3 players, laptop, game consoles).
81%. Percent of physicians will own a smart phone by 2012. Physicians are one of the highest using Smartphone demographics overall.
5,820. The number of health apps that were available for download from the major online Smartphone app stores (as of a report published Q2 2010).
66%. Percent of Americans who are interested in receiving health related emails from their health insurance company… 52% would be open to receiving emails that provide them feedback on their health process.
Is Slacktivism Good?
I guess it’s kind of like being an “arm-chair quarterback” or a “back seat driver”. Slacktivism (Slacker + Activism) refers to doing good without doing much. Donating thru a text message. Clicking on a link to generate donations. Wearing a rubber wristband to show your support of a cause.
Is this bad?
I don’t think so. Obviously, the world needs activist who actually roll up their sleeves and get involved in solving the world’s problems. But, are people that support them thru money (or clicks) or some other form of support not important?
In today’s social media world and connected world, donating and supporting causes should be easier. Everyone wants to announce their support for movements in Facebook from “my college is better than yours” (Go Blue!) to “I checked my H1c today” to “stop Communism”.
But, the article in Fast Company that got me on this topic talks about a few great case studies:
- FreeRice.com – For every correct answer you get to the questions they ask, 10 grains of rice are donated to the UN World Food Program. Why not? 22 million bowls of rice have been generated by this program.
- Haiti donations to the American Red Cross – The $10 text message pledges raised $38M.
So, how do we tap into this with healthcare? That seems to be the Holy Grail.
- Lose weight without diet or exercise. (why so many weight loss pills sell)
- Take my medication without having to remember every day. (e.g., patch)
- Track my vitals without going to the physician’s office. (connected devices)
Social pressure certainly plays a role here. The question is whether our privacy concerns outweigh the benefits (often not understood) of participating in certain social activities. For the younger generation, this will not be an issue. They don’t view privacy the same way. For the older generation (who by the way are the sick and expensive patients today), privacy is a big deal and some of them are technophobic (although probably less than you think).
BTW – Did you click thru on the FreeRice.com link yet? Come on.

Cluster Marketing and Communications Challenges
This is a term that a friend of mine introduced me to a few years ago. How do you coordinate messaging across channels and the timing of the delivery of those messages to drive a behavior?
- Do I send an e-mail and then call the individual if they don’t open it in 72 hours?
- Do I send a postcard before I send a letter?
- Do I call someone to tell them that I’m sending them an e-mail?
- Should all the messages be the same? Or should they show a progression of urgency (for example)?
- Do you have a single view of the consumer so you know what they have historically responded to?
- Do you manage your communications as an integrated process so once they take an action you can immediately stop the next communication (e.g., the patient logged into the website last night so don’t send the e-mail scheduled to go out in the morning)?
These things aren’t easy especially in healthcare where the technology to manage direct marketing is several years (being nice) behind consumer markets like banking or consumer goods. But, this is one thing that Silverlink Communications does for clients. Understanding these challenges, providing industry experts to design solutions and test plans, and having a technology platform to execute, track, and report on these challenges is what we do.
Another common challenge is determining frequency. Should I call the person once a day, once a week, once a month, or once a quarter? How is that different based on the result of the prior interaction? How is that different based on their condition? How is that different based on the drug they’re taking?
For example, I might call a patient recently diagnosed with depression in the initial few weeks to remind them to stay adherent with their medications as it may take a few weeks for them to feel a difference. For patients on drugs with immediate side effects, I might need an earlier intervention.
A few points from Dan Ariely, author of Predictably Irrational (Spirit Magazine, pg 46, July 2010):
- He observed that people doing work that involves decision making needed more positive feedback during the process. Do patients need more positive feedback for doing the right thing? Should you reach out and say good job for going to the physician?
- He observed that people lose motivation if the work they do goes unnoticed. Should companies call patients and say thanks for moving to mail order and saving them money?
- He observed that large rewards cause pressure which distracts from the task at hand. How do you break down your rewards into more near term reinforcement and don’t forget about non-monetary rewards?
- He observed that people are more committed to change when it’s there idea. How do you get patients to think about things they should do? One of his suggestions was to ask more questions.
But, this is only part of the challenge. How do the attributes of your intervention affect their likelihood to act? Could the name of your call center agent matter?
A study by the Edinburgh International Science Festival found that people make assumptions about people based on their names:
- People with royal names (James and Elizabeth) are assumed to be highly successful and intelligent.
- People with soft sounding female names (Lucy and Sophie) are assumed to be the most attractive.
- People with short male names (Jack and Ryan) are assumed to be more rugged.
If you’re using an automated call, does the voice talent you use matter? (see prior article)
Researchers at the University of Wisconsin-Madison found that a mother’s voice is as comforting as a hug which lowered levels of stress inducing cortisol and triggering the production of oxytocin (aka, the love hormone). [What’s a male’s reaction to their mother’s voice?]
And, of course, all of this has to be thought of from the patient’s frame of reference. Calling a recently diagnosed diabetic about adherence is very different than someone who has stopped taking their medications after 5 years. How do you treat them differently?
What about their current location? Is reading an e-mail on the blackberry during a commuter train different than reading it at your PC while eating lunch…YES!
This is why communications is a blend of art and science. You have to use data to drive fact-based algorithms which are adaptable in scale (i.e., across millions of people) and are adaptable as people, situations, and messages change.
How Blunt Should You Be?
I’ve talked about this before from my personal perspective so I found this article about shocking men into going to the doctors right on point. But, I think this begs a great question…
“Should you communicate differently with men and women?”
My short answer is yes. In reality, it doesn’t always make a difference, but there are lots of times when it does. I’m not sure I’m ready to bet the farm on shocking messages to men all the time, but I would love to try that. Imagine an adherence message that told them they were improving their likelihood of death by 27% by not taking their medications. Or, a message about going to get a prostate exam which pointed out how many people die per year.
Most healthcare companies keep the gloves on when delivering messages. They are trying to motivate them, but they are hesitant to be too blunt (or direct). I’m sure that generally makes sense, but sometimes you just have to catch someone’s attention to get them to act.
Telling someone they are overweight and should start to workout and diet is very different than saying they are obese and are likely to die in their 50s if they don’t change their lifestyle immediately.
Related story – Top 5 Reasons That Men Don’t Go To The Doctor
Growing Horns, Turning To Stone, and Other Random Diseases
We can all be a hypochondriac at some point in our lifes. Now, there’s a handbook for you to make you think about all the completely random diseases which exist.
– Get addicted to carrots
– Unintentionally speak with a foreign accent
– Believing you’re dead (Cotard’s syndrome)
– Constantly shocking other people
– Alien hand syndrome
– Stone man syndrome
– Guinea worm disease
– Human botfly myiasis
– Alice in Wonderland syndrome
Performance Guarantees from PBMs
This article appeared a few months ago, but I’m finally digging out. (Drug Benefit News – 12/4/09) It’s an interesting article about how some PBMs are using performance guarantees in their sales efforts. I would expect this to be a growing trend as the PBMs focus on outcomes and have a need to commit to those.
The article mentions that CVS Caremark offers performance guarantees in five areas – adherence, generic-drug utilization, preferred pharmacy choice, specialty drugs, and utilization management. The results are aggregated into one guarantee. There is apparently no charge to the client, but there is a penalty paid if the goal isn’t met. Seems like a good deal if the guarantees are aggressive enough to account for any pricing differences.
A consultant says that Medco also offers performance guarantees (but doesn’t offer any details). The consultant also says payouts range from $800 to $1,300 per patient who have the targeted condition, receive interventions, and don’t achieve the compliance target. That seems like a great incentive for participation to the plan and for the PBM to develop an effective program.
Some of the keys for good performance guarantees are:
- Good data (baseline and going forward)
- Clear metrics
- Comparisons to a control group and/or national metric (so you don’t just ride the curve of generic conversions for example)
- Long-term contracts
Member ID Card Application on iPhone
Priority Health (which I find to be a well run and progressive managed care plan) announced their new iPhone application. I suspect many will follow. It’s simple today, but imagine all the information you can put there – copays, drug history, lab values.
How Do You Pull, Push, and Pay?
I was reading something on Healthwise this morning. We recently had Don Kemper (CEO) present at our client event in May. He was talking about “Billion Dollar Decisions: Right Tools, Right People, Right Time”. A few key things from the overview:
- Today’s healthcare crisis can’t be solved with out helping everyone do more for themselves.
- People need to ask for the care they need and avoid care that’s not right. (a huge information and health literacy challenge)
- Every year people make 300M major healthcare decisions, 50M surgeries, 100M medical tests, and 150M+ major medication changes.
- Patient decision aids are key – http://ipdas.ohri.ca.
The summary was that to get people to uses decision aids you have to employ pull, push, and pay strategies.
Pull: Consumers pull the decision aids from the Web.
Push: Providers and payers push contextually relevant decision aids to consumers when they need them. (What Silverlink does!)
Pay: Providers and payers create incentives to encourage the use of decision aids.
Gender Bias – Postpartum Depression
We all know that females are different that males in terms of healthcare. And, regardless of the data, we all have biases in terms of what we believe. These biases can cause issues. (As I often say…”When you assume, you make an ass out of u and me.”)
That being said, I found the study a few months ago interesting where it said that 14% of American men develop depression either during their partner’s pregnancies or in the first year after delivery (peaking when babies are 3-6 months old).
This is important since depression is correlated with lots of health issues and has a family impact. The article mentions that children of depressed fathers have more emotional and behavioral problems than other kids at age 3 and more psychiatric disorders by age 7.
An interesting note was:
“Any healthy adult who goes without good sleep for a month is liable to become depressed.”
The big takeaway from the study is that physicians (and other healthcare entities) need to treat the family around birth. This is probably also a great opportunity for social media to support fathers as much of today’s infrastructure is set up to support the mother.
5 Keys To Health Plan Survival
I thought I would re-post these from the Corporate Research Group.
Bertolini outlined five keys to surviving reform: 1. Payment reforms that shifts incentives from volume to outcomes; 2. Information technology that improves quality, lowers cost; 3. Wellness: engaging consumers with incentives and decision-support tools; 4. Transparency tools that provide information and improve accountability; 5. Revamped benefits and plan designs.
These seem pretty logical and echo some of the things I brought up in my pharmacy white paper last year.
1. The need to better engage the consumer in understanding their benefits and ultimately responsibility for their care;
2. The effort to automate and integrate data across a fragmented system and across siloed organizations; and
3. The shift from trend management to being responsible for outcomes.
Pay For Full Service
In several industries (e.g., travel), you pay when you access a customer service representative. That forces you to use the self-service options of the Internet and/or the automated call line. Could this work in healthcare?
I doubt that people would be so directive as to penalize people for talking to a representative or a clinical person especially on such a sensitive and personal a topic as healthcare.
BUT, on the other hand, a disproportionate amount of calls are for mundane issues or questions would could be solved using other channels. The fact is that these channels have to be efficient and easy to navigate (which they aren’t always today). But, technology continues to become more ubiquitous so it’s not unreasonable to expect people to self-service more often.
One idea that I tried to sell years ago at Express Scripts was more around incentives for self-service. Why not offer large employers a discount if their use of the call center decreased? They have some opportunities to influence this. They could put a link to the website on their intranet. They could leverage their e-mail network to push out messaging. They could encourage people to use the PBM (or health plan) website.
On thing that several CFOs told me years ago was that they would frame the problem differently for their employees. It wasn’t about just saving money to reduce cost, but it was about re-directing funds to cover more things. For example, one company had to cut $10M in expenses. They were looking at plan designs to accomplish some of that. But, they also thought they were going to have cut on-site daycare. We looked at one strategy that might save them $15M so they could achieve their savings and actually grow both the daycare program and their 401K matching program.
What great positioning to the employees! Here are two things we are going to give you…all you have to do is help us shift costs from point A to point B by taking the following actions.
New Health Insurance Ideas
Just two ideas that I was playing with for health insurance.
1. Complete transformation from group to individual
Why not change the entire market to be an individual purchase…There are obviously some reasons such as adverse selection and group buying power, but I would think those were things where the government could add value. If individuals selected the health insurance companies and products that they liked, it would create a very different dynamic.
You could then change the employment paradigm not to a provider of health insurance, but make it more a part of your compensation. Company A might fund up to $5,000 per year in health insurance while Company B provides up to $7,200 for family coverage.
One of the big benefits of this (beyond making individuals into consumers with power) is that health insurance companies could start to invest in outcomes. Today, they are hesitant to make long-term investments (i.e., if I do this for 5 years, it will reduce the cost of this individual in 20 years) because their membership turns over. This is a real issue in my mind.
2. Free insurance for healthy people
There is obviously an issue with funding and hyperbolic discounting, but what if we simply said that people who maintain some set of health standards (BMI btwn 20-25; HDL less than 180; able to run a mile in under 8 minutes) got free health insurance. Would that make a difference? I think so. Companies would be better off – less absenteeism. The US healthcare costs would drop.
Of course, it would take it’s toll on the providers while being a boom for gyms. But, it’s hard to find that win-win-win.
I know there’s a big issue of funding, but I was thinking about some radical ideas of what the money being raised by Gates and Buffet could be used to do and how it could motivate people.

 August 7, 2010
August 7, 2010