I just finished the book Drive by Daniel Pink. It’s a great book. I’d recommend it from both a personal and professional perspective because it challenges so much of what we normally think. But, it’s both logical and based on tons of research.
He lays out three reasons why people act:
- Food, water, or sexual gratification (Motivation 1.0)
- Rewards and punishment (Motivation 2.0)
- Intrinsic reward (Motivation 3.0)
The concept of intrinsic reward was new to people. The concept of having this drive challenges all which we believe around incentives. And, his examples reinforce this point. People performed worse on certain tasks when a clear reward was identified.
“When money is used as an external reward for some activity, the subjects lose intrinsic interest for the activity.” Edward Deci
He uses open source collaboration as a great example of this. His example is whether you would have expected Encarta , an encyclopedia by Microsoft, or Wikipedia to succeed. Why wouldn’t a big company with unlimited resources beat out a collection of volunteers?
Business today is based on the whole concept of Motivation 2.0 (i.e., carrots and sticks). He talks about the historical presumption that absent some reward or punishment that people are inert.
“Enjoyment-based intrinsic motivation, namely how creative a person feels when working on the project, is the strongest and most pervasive driver” Lakhani and Wolf
He goes on to explain the difference between algorithmic and heuristic problems. Algorithmic problems can be solved based on a single path while heuristic problems have different options. [It’s like when I went to business school and architecture school.] He quotes a McKinsey study which says that 70% of job growth in the US is around heuristic work. Therefore, applying a traditional model of motivation to creative work creates a major issue. It turns creative work which we feel passionate about into a disutility (something we won’t do without payment).
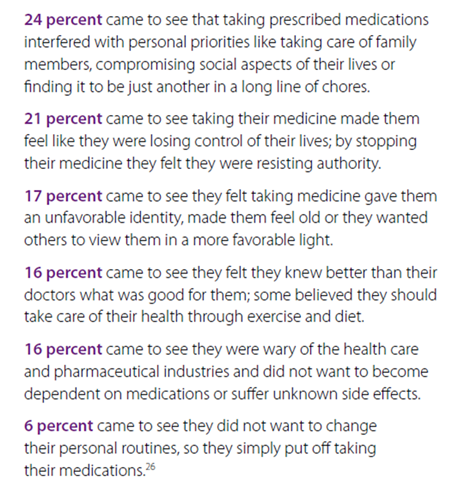
Now of course, creative “work” isn’t “play” if the basics aren’t addressed – i.e., fair pay. This has application in lots of areas including how we get kids to learn. Paying kids for specific activities pushes them to focus on completing those but not necessarily learning how to apply the knowledge. I think it’s a key issue which should be getting debated in when, if, or how to use incentives in health care. This is why you may see a short-term improvement that falls off over time.
This will be very relevant as P4P becomes more important. If rewards narrow the focus of solutions and limit creativity, will that be good in that it focuses people on specific processes? Or will it be a problem because in complex cases or cases where there are alternatives, the creativity of solutions and consideration of options will be limited?
But, he’s careful to make sure you don’t think that rewards are always bad. They have to be used appropriately and for the right tasks.
“If we watch how people’s brains respond, promising them monetary rewards and giving them cocaine, nicotine, or amphetamines look disturbingly similar.” Brian Knutson
He lays out “The Seven Deadly Flaws” of using carrots and sticks:
- They can extinguish intrinsic motivation.
- They can diminish performance.
- They can crush creativity.
- They can crowd out good behavior.
- They can encourage cheating, shortcuts, and unethical behavior.
- They can become addictive.
- They can foster short-term thinking.
He suggests that for tasks that don’t inspire passion nor requires deep thinking that there are three things that are important:
- Offer a rationale for why the task is necessary.
- Acknowledge that the task is boring.
- Allow people to complete the task their own way.
He talks about how using bonuses can work even for creative tasks when it’s not an “if-then” reward, but it’s a “surprise”. (Which is hard to repeat multiple times.)
He goes on to talk about Type A personalities. Theory X and Theory Y. Type I and Type X. It makes some key points about how we perceive people. Do we believe in the “mediocrity of the masses” or do we believe in people’s interest in succeeding? This is where Motivation 3.0 begins to come in and there is a focus on people’s desire to success or to master something.
He makes a lot of points that remind me of Malcolm Gladwell’s book Outliers. Mastery is hard work.
“The most successful people, the evidence shows, often aren’t directly pursuing conventional notions of success. They’re working hard and persisting through difficulties because of their internal desire to control their lives, learn about their world, and accomplish something that endures.” (pg. 79)
He talks about how these frameworks can be applied at an organizational level and cites a Cornell University study of 320 small businesses. Those that offered autonomy grew at four times the rate of control-oriented firms and had one-third the turnover. He talks about ROWE (Results Oriented Work Environment) and gives examples of companies that really give their employees freedom. It’s a radical change for many people…imagine a work environment where you set your own hours.
He introduces the concept of “flow” from work by Csikszentmihalyi which was new to me. It describes this state where people are challenged but have an opportunity to stretch to get there.
He talks about mastery as a mindset and how what people believe shapes what people achieve. This belief is critical especially in addressing things like obesity (my opinion) and plays into a lot of what you see on The Biggest Loser. Losing weight (mastering being in shape) is a lot of work, and you have to believe you can do it. You also have have to have some motivation other than financial goals.
There is an interesting discussion of “entity theory” versus “incremental theory” which talks about whether you believe you have a finite intelligence or an opportunity to expand your intelligence. There is lots of talk about education in the book which I think is really important. Are we creating kids that want to “prove their smart” by getting A’s or who are really trying to learn?
“West Point grit researchers found that grittiness – rather than IQ or standardized test scores – is the most accurate predictor of college grades.”
He has a whole chapter on purpose. I think this is key to healthcare. He talks about autonomy and mastery, but without purpose, we don’t have balance. Think about someone who is obese. They want to be autonomous and master being in shape, but when you listen to them talk, it is typically a focus on being there for their family that motivates them to actually take action.
He made me wonder about linking health outcomes to lower costs (i.e., value based). If I know that my healthcare premiums go down if I manage my BMI or cholesterol or get certain tests done, am I just checking a box or am I really changing my lifestyle in a sustainable way?

 April 6, 2011
April 6, 2011