Rebecca from ProjectHEALTH closes #results2010 with a remarkable talk on this crucial program; they work with 5,000 families/year.
Reid Kielo, UnitedHealth: 93% of members validated ethnicity data for HEDIS-related program using automated telephony #results2010
25% of Medco pt take a drug with pharmacogenetic considerations. Robert Epstein, CMO Medco #results2010
Bruce Fried: the “California model” of physician groups facilitate efficiencies that improve delivery; an oppty for M’care #results2010
Bruce Fried on Medicare: 5 star ratings have strategic econ. importance, med. mgt. and cust serv. key #results2010
Fred Karutz: members who leave health plans have MLRs 2 standard deviations below the population. #results2010
Fred Karutz: Market reform survival – retain the young and healthy #results2010

 Poly-pharmacy has negative impact on adherence. #cvscaremark
Poly-pharmacy has negative impact on adherence. #cvscaremark
#results2010
1 in 3 boys and 2 in 5 girls born today will develop diabetes in their life. SCARY! #results2010
20% of all HC costs associated with diabetes. #results2010. What are you doing to manage that?
Messages to prevent discontinuation of medication therapy far more effective than messages after discontinuation. CVS #results2010

 25-30% of people who start on a statin don’t ever refill. #CVSCaremark
25-30% of people who start on a statin don’t ever refill. #CVSCaremark
#results2010
Maintenace of optimal conditions for respiratory patients increased 23.4% with evidence-based plan design. Julie Slezak, CVS. #results2010
Value-based benefits help control for cost sensitivity for medications; every 10% increase in cost = 2% – 6% reduction on use. #results2010
Pharmacists who inform patients at the point of dispensing are highly influental in improving adherence. William Shrank #results2010
The game of telephone tag in HC is broken. Pt – MD communications. #results2010
37% of Pts were nonadherent because they didn’t know they were supposed to keep filling Rx. #results2010
Last mile: 12% of Americans are truly health-literate; they can sufficiently understand health information and take action. #results2010
Only 12% of people can take and use info shared with them. #healthliteracy
#results2010
#DrJanBerger.
We need to improve the last mile in healthcare… clear, effective conmunication. Jan Berger #results2010

#McClellan used paying drug or device manu based on outcomes as example of “accountable care”. #results2010
72% of those with BMI>30 believe their health is good to excellent; as do 67% of those w/ chronic condition. #McKinsey
#results2010
Are incentive systems more likely to reward those that would have taken health actions anyways (i.e., waste)? #McKinsey
#results2010

 Only 36% of boomers rate their health as good to excellent. #results2010
Only 36% of boomers rate their health as good to excellent. #results2010
27% of people believe foods / beverages can be used in place of prescriptions. #NaturalMarketingInstitute
#results2010
Why do we spend so much time on impacting health outcomes thru the system when that only explains 10%. #Dr.JackMahoney #results2010
Using auto calls vs letters led to 12% less surgeries & 16% lower PMPM costs in study for back pain. #Wennberg
#HealthDialog
#results2010
MDs are much more likely to discuss pros with patients than cons. #Wennberg
#HealthDialog
#results2010
Should physicians be rewarded as much for not doing surgery? How do economics influence care decisions? #results2010
Physicians were 3x as concerned with aesthetics than breast cancer patients in DECISIONS study. #results2010
Fully-informed patients are more risk-averse; 25% fewer of informed pts in Ontario choose angioplasty. #results2010
Patients trust physicians over any other source (media, social connections) but only receive 50% of key knowledge. #results2010
Informing Patients, Improving Care. 90% of adults 45 or older initiate discussions about medication for high BP or cholesterol. #results2010
What is #results2010? #Silverlink client event.
#results2010 – #Aetna Medicare hypertension program leads to 18% moved from out of control to in control using auto calls (#Silverlink) …
About 2 of 3 medicare pts have hypertension. #results2010
John Mahoney describes how he connects payors, providers, and care via research. #results2010
As information becomes commoditized in healthcare, sustainability enters the vernacular. #results2010
Segmentation innovations of today will be tomorrow’s commodities. Measurement and learning must be “last mile” IDC insights #results2010
Plans are strategically investing in bus. intel to reach wide population for wellness, not just the low-hanging fruit. #results2010
The single most significant future market success factor is measurable results. Janice Young, IDC Insights. #results2010
Knowing our attendees’ preferences could have fueled segmented, precise invitations to #results2010. Dennis Callahan from Nielsen Media.
Drivers of those sereking alternative therapies: stress, lack of sleep and energy, anxiety, inflammation. #results2010
Only 2% of people don’t believe it’s important to lead a healthy lifestyle. Their behavior could’ve fooled me. #results2010
Are purity and simplicity the new consumption? Steve French of Natural Marketing Institute explores. #results2010
Gen Y is the most stressed out generation. #results2010
Less is more. 54% say having fewer material possessions is more satisfying. Natural Mktg Institute #results2010
Loyalty is a result of a cumulative set of experiences. Individual intervention ROI is sometimes difficult. #results2010
Sundiatu Dixon-Fyle of McKinsey; understand how beliefs shape an individual’s ability to change behavior. #results2010
Don Kemper: each of 300M HC decisions made each year need to be informed. #silverlink
#results2010
Medicare Part D: 40% lower cost than projected, seniors covered through tiered coverage powered by communication. #silverlink
#results2010
Mark McClellan: Brookings is engaging private insurers to pool data to understand quality of care. #silverlink
#results2010
Mark McClellan at RESULTS2010; bend the curves, provide quality care efficiently. HC reform >> insurance reform. #silverlink
#results2010

 June 21, 2010
June 21, 2010 

 Poly-pharmacy has negative impact on adherence.
Poly-pharmacy has negative impact on adherence. 
 25-30% of people who start on a statin don’t ever refill.
25-30% of people who start on a statin don’t ever refill. 


 Only 36% of boomers rate their health as good to excellent.
Only 36% of boomers rate their health as good to excellent. 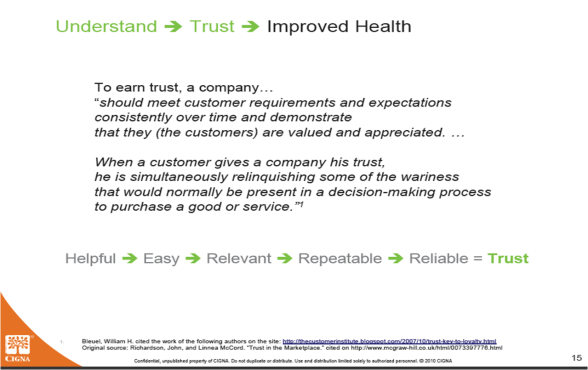





 The big changes they felt were bound to happen were cuts in Medicare and an expansion of the SCHIP program, and there were others that they said would be debated including being able to sell insurance across state lines, the government offering coverage, individual coverage mandates and coverage for pre-existing conditions. But the biggest part of the discussion was around healthcare costs. Costs that are out of control, who pays for services, and where will the money come from. While at an aggregate level talking about healthcare’s spiraling costs is simple, it is not the heart of the issue.
The big changes they felt were bound to happen were cuts in Medicare and an expansion of the SCHIP program, and there were others that they said would be debated including being able to sell insurance across state lines, the government offering coverage, individual coverage mandates and coverage for pre-existing conditions. But the biggest part of the discussion was around healthcare costs. Costs that are out of control, who pays for services, and where will the money come from. While at an aggregate level talking about healthcare’s spiraling costs is simple, it is not the heart of the issue.




