Medical Technological Innovations in Our Future
The history of medicine is full of technological innovations. The ECG in 1913, the Band-Aid in 1920, the cardiac pacemaker in 1950, CAT scans in the 1970s and the completion of the Human Genome Project on 2003 are just a few of the many inventions in just the last century.
Yet, we are now standing at a threshold of medical technological change unparalleled in history. In the next 20 years of the Shift Age, there will be more technological change than in the last 100 years. Let’s take a look, in loose chronological order at these changes of the future.
Low Cost Personal Genetic Mapping
In 2013 we will be able to have most, if not all, of our personal genetic maps completed for under $1,500, an outgrowth of the Human Genome Project. This is very significant as the knowledge each of us will learn from our individual genetic maps can help us act in a preventative manner. If, for example you are in your twenties and you find out that you have a genetic disposition to early onset Alzheimer’s, you can spend the next few decades doing whatever current medical wisdom says might slow the onset of Alzheimer’s; taking Omega-3 fish oil, working out every day and other discoveries about the disease. In other words, personal genetic maps will allow us to address whatever genetic dispositions we might have, BEFORE they happen to us!
Bionics
There are incredible developments in the area of bionics and replacement “parts” for the human body. New artificial arms and legs can now be controlled by thought and brain-waves. These are now being tested on veterans of the Iraq and Afghanistan wars. In the next few years there will be replacement eye-balls that will provide 20/20 vision for years. There will be ear implants allowing deaf people or people who have lost a significant part of their hearing to hear clearly again or for the first time. In the next decade we will develop replacement parts that are better than the “parts” we were born with!
Tissue Regeneration
Recent breakthroughs in stem cell research are pointing the way towards tissue regeneration for all of us. In the years ahead we will be able regenerate organs. This will lead us to each have the opportunity to regenerate organs from our own tissue, eliminating both the need for an organ donor and the possible rejection of the new organ that often happens. This will not be inexpensive, but it will be possible in the next decade.
DNA Pharmaceuticals
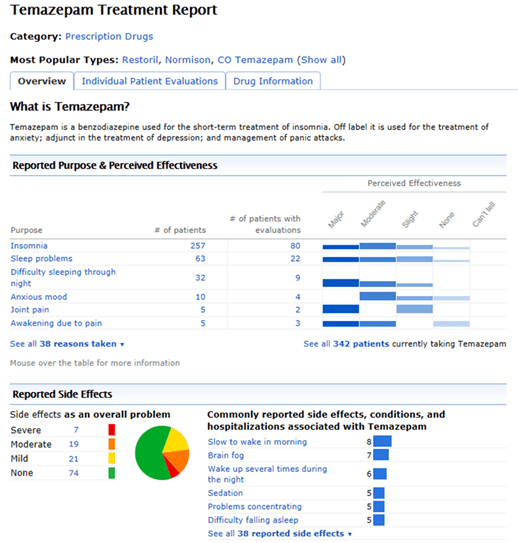
The technology for the development of DNA Pharmaceuticals flows from the ability to map individual’s genetic maps. Think of them as personalized drugs. We are all familiar with the “lowest common denominator” drugs as we see them advertised all the time. This great pill will lower your blood pressure, but it might also cause sudden death syndrome, erectile dysfunction, or loss of sight. With ever more precise genetic information, drugs in the future will be personalized to each patient, eliminating these horrible side-effects. What works for one person will not work for another and this reality will be finally addressed in pharmaceuticals.
Nanotechnology
A nanometer is a billionth of a meter. A human hair has a diameter of approximately 50,000 nanometers. Medical science is currently creating microscopic bots that can enter and move freely within the human body. The early use of this technology will be to directly attack cancers in the body with transported DNA-customized chemicals. Nanotechnology will allow us the ability to precisely deal with such cancers and not degrade the entire body with chemotherapy
Human Cloning
In the last two decades animals have been successfully cloned. This history, combined with some of the breakthroughs listed above, make the possibility of human cloning a reality by 2020, if not before. The real questions here are of course moral. What to do with experiments gone wrong? How to treat experiments gone right? The history of human and religious morality will be confronted with this real possibility. It will be able to be done, but will we want it done?
Guest Post written by:
David Houle is a futurist and author of the highly regarded blog Evolution Shift. He is the author of The Shift Age and The New Health Age, and a contributor to O The Oprah Magazine, The Huffington Post,and NPR. Houle spent more than 20 years in entertainment, as part of the executive team that launched MTV, Nickelodeon, VH1 and CNN Headline News. A sought-after lecturer, he was recognized as Speaker of the Year from Vistage International, the leading global organization of CEOs. Houle is Futurist in Residence at the Ringling College of Art + Design in Sarasota, Florida.

 January 19, 2013
January 19, 2013