I think this is a question many of my PBM friends would like to know. Fortunately, a few of the Walmart people that read my blog and are part of their Health and Wellness group agreed to sit down and talk about their strategy.
Let’s start with setting some background:
- Walmart was the first to introduce the concept of $4 generics which originally caught the market off guard and has created lower generic costs and free antibiotic programs at several pharmacies. [I would also argue that it highlighted the fact that generic copays were getting too high.]
- Walmart was the first to work directly as a pharmacy to create a limited network contract direct with an employer (Caterpillar).
- Walmart has partnered with Humana on a limited network offering for Medicare.
- Walmart came out with a direct to consumer mail order pharmacy offering.
If you follow the industry, you know that all of these things were potential game changers (if they’ve worked).
This creates some tension:
- Is Walmart simply a catalyst for change in the healthcare space?
- Does Walmart (pharmacy) want to disintermediate the PBM?
- Is Walmart able to make money where others can’t?
- Does Walmart get more foot traffic such that pharmacy can be a loss leader?
Here is the Q&A [interpretive not literal] from my dialogue with Marcus Osborne (Sr. Director, Business Development, Healthcare, Walmart) and Tom Hill (Director, Health Services Development, Walmart).
What is Walmart’s Health & Wellness strategy?
Walmart wants to help consumers “save money and live better”. That is our DNA and our fundamental approach to the market. Pharmacy has presented a unique challenge since consumers often have the same copay regardless of which pharmacy they went to. Even when it’s a percentage copay, the savings differential might not be much to the consumer. Walmart was disconnected from the consumer in the traditional pharmacy pricing approach. That has driven us to look at unique ways that we can create savings.
How does Walmart decide what “offerings” to bring to market?
Walmart looks at ideas that focus on our EDLP (Everyday Low Price) concept and leverage our supply chain efficiencies. We are constantly looking at non-store operational opportunities to work directly with key companies. We currently have over 20 direct relationships with managed care companies and PBMs where we are working with them to drive down consumer costs in the pharmacy and broader healthcare area.
Obviously healthcare is bigger than pharmacy. What other things are you doing to drive healthy eating, management of critical conditions, or other programs? We’re constantly looking at what’s needed in the healthcare sector and where to invest. We focus on our two key advantages:
- Willing to trade profit for volume
- Value of the total “box” [store]
A good example is the work we’ve done around “Healthy Mom Healthy Baby” in Medicaid. We looked at the issues of high pre-term labor and the high rates of injury post-birth. We felt like we had a moral and cost imperative to take action. As part of this, we worked with several managed care groups to redefine the entire process and look at our unique assets. Our solution includes:
- Free pregnancy tests
- Free pre-natal vitamins
- Rewards for free diapers and other supplies tied to physician visits and other health activities
- Free car seats
- Leveraging our physicians and clinics
[I was impressed…this was a broad solution that looked at a lot of their assets.] We’ve also created several diabetic specific solutions; a smoking cessation program with Healthways; weight management programs; and women’s and men’s health programs. The focus is on payers that are at risk for their healthcare spending with more to come from clinics.
Will Walmart become a PBM?
No. We’re not looking to go into the PBM market. We’re supply chain experts. We see value in the PBM model. [We talked a little about the fact that “you are what your profits say you are” meaning that the PBMs have painted themselves into a profit corner where their profit comes from generics at mail order so any threat to that is a challenge.]
If the Caterpillar model was so successful, why haven’t others adopted it?
The reality is that over 400 employers have contracted directly with Walmart for a limited network model similar to Caterpillar. They are all seeing significant savings.
Does Walmart see the market through “different glasses” than others?
No. We still want to have the pharmacy be a profit center. We’re not looking to bottom out the market, but we are willing to trade lower profits per transaction in return for more market share. At Walmart, it’s not about maximizing revenue/Rx or profit/Rx…it’s about total revenue and total profitability. [A very different strategy than other CFOs which would say you can’t expect volume to make up for lower profitability.] Obviously, we also have the opportunity to get non-pharmacy sales associated with food traffic. One thing that may be is different is the fact that we believe scale should drive down costs. In pharmacy, the biggest players are always trying to command a premium. We think it should be the other way around. We also have been able to get our cost-to-fill to be the same at retail and mail so we’ve become channel ambivalent.
Have these programs improved market share in any significant ways? You have to look at the programs separately, but overall we’ve seen our market share increase from 6% overall [when the $4 generic program launched] to 10% now. The network design strategy has had great success. We look at three types of programs:
- Incentive based networks
(Caterpillar 1.0) where all the pharmacies are in the network, but there is a lower copay to go to certain pharmacies. If only 15% of pharmacies are preferred, their market share doubles. If Walmart is the only preferred pharmacy, their market share goes up 4x.
- Limited networks where some pharmacies are removed from the network. If you drop the network significantly, they’ve seen their share go up 2-3x.
- Limited networks with preferred pharmacies where you some pharmacies are removed from the network, but within the remaining pharmacies, there are still incentives to go to certain stores (Caterpillar 2.0). In these cases, they’ve seen their share go up 10x.
The $4 generics program has helped increase market share by an estimated 150 basis points. In many cases, companies that initially jumped to offer similar programs have dropped them. They couldn’t sustain them.
The Medicare program with Humana has been very significant and successful [as demonstrated by Humana’s huge jump in Medicare lives].
The direct-to-consumer (DTC) programs for mail have been pretty limited and haven’t had a huge impact, but they’ve been offered in markets where we have no stores (e.g., Detroit and NY) and therefore almost no share to begin with so any share is a gain.
People complain about the pharmacy location within the store. Would you ever consider a direct access point to the pharmacy which didn’t involve going through the entire store? This is a very hot topic. We did a lot of research about store design and what goods should be located next to each other, but in the end, we’re considering moving the pharmacy closer to the front entrance. Right now, 25% of the stores have a drive-through pharmacy which gets utilized at a very high rate. But, this does lose the pharmacist face-to-face benefit. [At the end of the conversation, my take is that they are looking at lots of scenarios here and trying to figure out the balance of convenience to the pharmacy only consumer and how to optimize the entire footprint.]
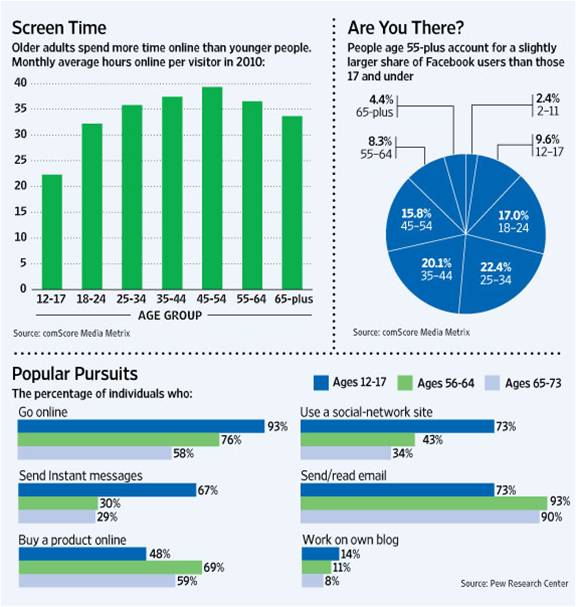
The partnership with Humana really seemed to help them grow their Medicare lives this year. How did this come about? We both were looking for new solutions to leverage the fact that scale matters and how to operate within the CMS parameters. We felt like there was an opportunity to do something different and began speaking with plans about some limited network ideas. We know that Walmart is over-indexed in the 65+ category based on store visits per week. Based on that, we were looking at what we could do to offer them more value as compared with our traditional, core customer of 35-50 year old females. Through a series of conversations, the partnership was born. We’re very happy with the relationship and believe they are also.
Limited networks have been around for a long-time with limited adoption. Do you think their time has finally come? What has changed? They have been around, but historically the networks weren’t limited enough to create enough savings to overcome the “costs” of disruption to the payer. Based on our experience at Caterpillar, we believe that you will see a transitional period where companies first move to incentivized networks and then 1-2 years later move to limited networks. [Something I would compare to the transitions which have happened in formulary over time.] The one area where we do see limited networks happening more rapidly is in the area of Managed Medicaid. [This plays into the focus of PCMA and others on the PBM opportunity around Managed Medicaid.]
It was a great discussion. I learned a lot. They allowed me to ask them a lot of questions about their programs and approach that honestly had led to some skepticism in the past. It sounds like they’ve brought together a great team with a broad vision of what they can do in pharmacy and in health and wellness overall. It has gotten my mind thinking about ideas, and I look forward to learning more.
[BTW – You can sign up to get posts like this e-mailed to you whenever I write them. A registration link is in the right hand column.]

 October 22, 2011
October 22, 2011