There was an interesting story which came out of Michigan this past week from Christy Duffy about how her physician’s office was requiring all minors between the age of 12-17 to have a 5 minute private conversation with them (according to the law). Of course, it appears that they made a mistake per her later post, but I think it serves to make several interesting points.
1. Don’t always assume that someone’s interpretation of the law is right if it doesn’t make sense. Sometimes, you have to apply common sense and push back or ask questions.
2. There is a gray area between protecting the rights of our kids and protecting our rights. While the intent of allowing our kids to have honest and open conversations is appropriate, there needs to be some involvement of the parents.
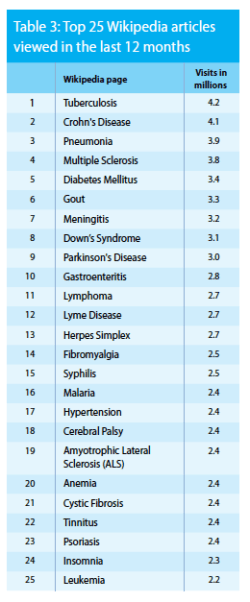
It’s an interesting topic for discussion. Should our teenagers have access to providers on their own? Yes. If a teenager has a health issue, I think we’d all prefer that they talk to a professional rather than Dr. Google or their friends to find the answer.
Should a provider be able to force a private conversation with a minor? Yes…if they have a legitimate concern about abuse, but I don’t see any other reason.
Should a teenager who’s covered by my insurance and lives in my house be able to block me from having access to their medical records? Yes. This is the law, but should providers be having private conversations to offer them this option? I don’t think so. I would like them to have those discussions with me and my child to say that here are their options.
Should a teenager have a private conversation with their provider about STDs, HIV, and birth control? Yes, BUT I’d like to have the conversation at the right age with me in the room initially and then offer the private option. I don’t think forcing that conversation on a 12-year old would make sense in a private setting.
Ultimately, this comes down to the issue of access to the medical records online. What I heard was that this would also require the provider to get a cell phone and e-mail address for my kids. Obviously, if they’re doing something confidentially with the doctor, that’s one thing, but as a matter of record, I disagree. (I don’t even give out my kid’s Social Security numbers.) I don’t want my kids to start getting e-mails, phone calls, and letters sent directly to them as early as 12-years old. And, yes…I do try to shelter them a little. We talk about all the issues, but in a way that my wife and I want them to learn, not according to some formula driven approach that’s mandated. But, ultimately, I don’t think a 12-year old is mature enough to make all their own health decisions or to feel like they should.
Obviously, some part of this falls on the parent regardless to create an environment of open dialogue with their kids. The kids have to feel comfortable talking with their parents which is important for health and many other challenges that our kids have to deal with. And, unfortunately there’s always bad people in any profession so while sexual abuse by a physician or nurse is rare it’s not unheard of. Ideally, I think you should have the choice of when to encourage a private conversation and never have it mandated (unless of course the provider suspects abuse). Unfortunately, with a report of abuse being made every 10 seconds, we have a huge problem in our country.

 July 10, 2014
July 10, 2014